This isn’t directly related to nutrition, but this question has come my way, so I am happy to talk about it. This question comes up for dietitians working in diabetes and renal care because when metformin gets stopped, blood glucose levels increase. This prompts the nutrition consult!
What is the recommendation for Metformin related to kidney function?
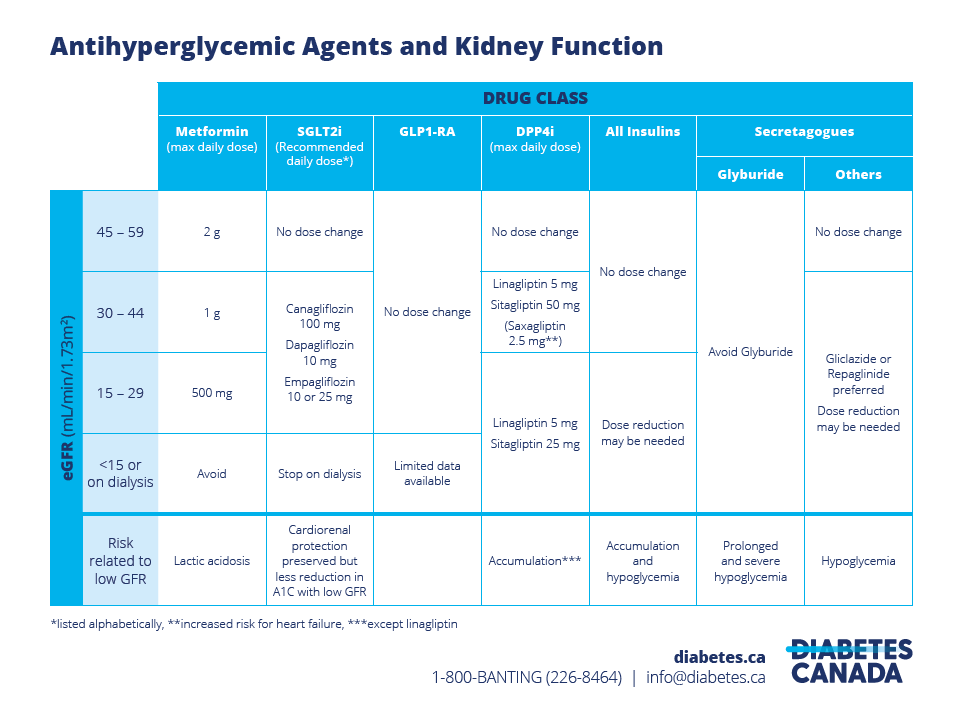
According to the Diabetes Canada Renal Dosing Chart, prescribers should avoid metformin when the eGFR goes below 15 or for those on dialysis. The risk reason identified is Lactic Acidosis.
Does metformin harm the kidneys?
Many patients have told me that metformin was stopped due to kidney harm, but this is incorrect. The reason for stopping Metformin is the risk of lactic acidosis. Metformin is not linked to an elevated risk of kidney function decline.
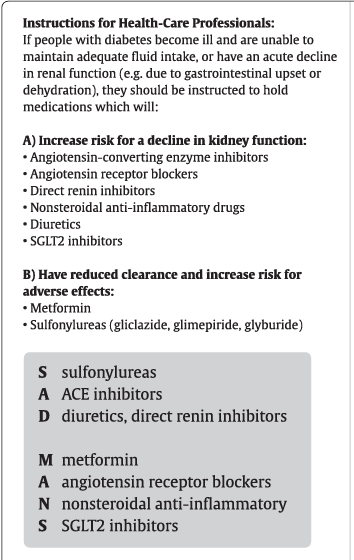
Check out this Sick-Day Medication List (again from diabetes Canada). Notice that ACE-inhibitors, ARBs, NSAIDs, Diuretics and SGT-2s are all under the increased risk of kidney function decline (kidney injury) but metformin is under the heading of increased risk of adverse effects.
What is lactic acidosis?
Ok if the risk related to metformin and kidney function is lactic acidosis, then the next reasonable question is – what is lactic acidosis?
According to Medline, excess lactic acid in the blood stream can lead to lactic acidosis. It can cause nausea, vomiting and weakness. After intense exercise, you may have experienced mild lactic acidosis, also known as sore muscles!
What is the history with lactic acidosis and metformin?
According to this 2021 case-control, the original concern with metformin and lactic acidosis actually started with metformin’s predecessor, phenformin. In 1977, phenformin was taken off the market. At that time biguanides had a label-warning against use in the creatinine was greater than 1.5mg/dL for men and 1.4mg/dL for women.
In 2016, the FDA updated the regulations for metformin. New evidence suggested that the risk of lactic acidosis was low until the eGFR was less than 30.
How common is lactic acidosis?
Using data from the same 2021 article, they looked at people who had filled a metformin prescription within the last 3 or 6 months and who had lactic acidosis. They matched them similar people who did not take metformin (the control group).
They had 2791 people taking metformin and 26 473 controls. The number of lactic acidosis events was 227 for those on metformin and 2385 for the controls. Because they had data on these groups for several years, they also calculated the total number of years they followed each person and added them up. The had 5665 years of follow up for the metformin group and 60984 for the control group.
Then they calculate the incidence rate. The incidence rate for the metformin group was 2.01 per 1000 patient years. For the control group it was 1.96 per 1000 patient years. The 95% confidence intervals overlapped.
When they broke down the results by CKD stage, they reported that as eGFR declined, the hazard ratio of experiencing an event (lactic acidosis) increased.
Ok, so what does this mean? Lactic acidosis is relatively uncommon, there will only be about 2 events for every 1000 person years. It is slightly more common in those people who take metformin and those with lower kidney function are at higher risk. But again, the absolute rates are low.
Take Aways
- Metformin does not cause kidney damage.
- Metformin increases the risk of lactic acidosis. But, even people who aren’t taking metformin have a risk of lactic acidosis.
- Rates of lactic acidosis are low.
- For people on metformin, who have lower kidney function, they have a higher risk of lactic acidosis.