Today’s journal club article: Experiences and Perspectives of Dietary Management Among Patients on Hemodialysis: An Interview Study
Background
For those of us who work in renal nutrition, we know that the renal diet is challenging.
This article, interviewed adults on HD to try to assess barriers and facilitators to adopting a renal diet. I was surprised to read that diet is the least “compliant” aspect of patient care. When compared to following dialysis schedules or taking medications. Well, maybe not surprised perse. But, interested in thinking that of all the things we ask patients to do – come to dialysis, take medications, change what you eat, etc, etc that changing what you eat is the hardest part.
Methods
This study was conducted in 6 dialysis units in Australia using a semi-structured interview tool.
I checked out the questions and I thought they were pretty good. These are certainly questions I would love to have the answers for to help me with my work.
The interview questions
- Can you tell me briefly about when you started haemodialysis. What do you think were the
biggest changes since starting haemodialysis?
General beliefs about diet and lifestyle - Can you describe your experience with diet and lifestyle changes after starting on haemodialysis?
- How well do you think you are eating? And why.
- In the context of managing all aspects of your haemodialysis treatment (medications, dialysis etc) on a scale of 0 (not important at all) to 10 (most important), how would you rate the importance of diet in managing your disease and why?
- How do you manage your different dietary needs?
- What component/s of your diet do you consider most important and why?
- What do you think is the most/least challenging part of lifestyle (diet, physical activity)
management for you to deal with? And why. - On a scale of 0 (not confident) to 10 (extremely confident) how confident do you feel in being able to make the right dietary choices – why?
- Has there been a time when you have been able to change an aspect of your diet or lifestyle? If
so, what strategies helped you achieve this change? And why. - What aspects of your dietary and lifestyle management do you feel you need more education or
support? - Can you suggest some things that might help you to change behaviours, particularly related to
nutrition and physical activity? - How do you like to receive information or education about nutrition and lifestyle? And why.
- How often would you like to be counseled regarding diet and lifestyle? And why.
- Who do you think is the best health professional to give you diet and lifestyle advice? And why.
The Results
The authors highlight two key barriers and two key facilitators to following a renal diet. They created a beautiful figure to help tie it all together.
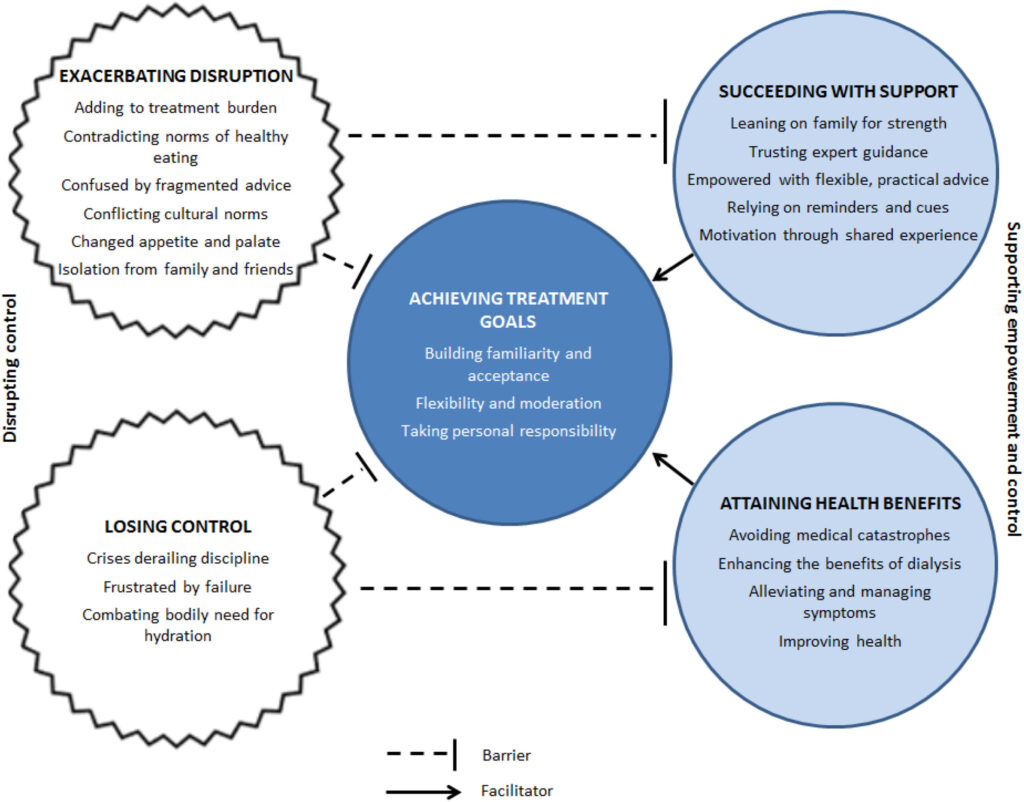
Barrier: Exacerbating Disruption
My key take away from this barrier is the overwhelming nature of starting dialysis. The authors state that for many people it gets easier over time. As a clinician in the area what I worry most about is patient’s getting given conflicting advice and how this creates a barrier to adoption. One of the quotes in the paper said they saw three different dietitians who said three different things.
I think one of the challenges that creates problems such as conflicting advice is often the lack of evidence and information about foods that will actually have an impact on patient outcomes. We have a lot of work to do on this one before this gets better I think!
Barrier: Losing Control
Here the authors describe trying to manage life and relationships in addition to health is daunting. They also highlight that patients can feel frustrated when they work really hard to be compliant with diet recommendations but the blood work results don’t improve.
I see this a lot. Even today, I spoke with someone has ongoing chronic hyperkalemia. They are following the low potassium diet but the potassium is still high. My goal was to explain that there can be factors beyond diet that impact potassium levels. But, it was a hard sell! I think this also comes back to a lack of evidence supporting our diet recommendations. This makes it difficult to give the right advice. I also see it happen when diet is sold as the “cure-all” by members of the health care team.
Facilitator: Achieving Health Benefit
A faciliator was the perception that changing their diet resulted in benefits to health, Or improvements in their symptoms. Hooray! This one feels more positive. When the advice we give works, patients feel better and they want to keep following the advice.
Though, again I think this loops back to those evidence-based interventions that can actually be associated with improvements in health. Which, sometimes feel like is few and far between!
Facilitator: Succeeding with Support
Overtime, patients reports that they get used to the renal diet and start to see it their normal diet. They also reported that regular contact with the dietitians enabled them to get the individualized nutrition information that they needed. Patient’s also talking about the importance of supportive family and the dialysis community to help them.
Discussion
I liked this little article. I thought it did a nice job of summarizing the barriers and facilitators that help with dietary adherence.
To help reduce barriers, I wonder about providing more education to my colleagues about the importance of nutrition. And, referral to a dietitian to provide nutrition education. Hopefully if more nutrition advice is coming through the dietitian then the message will be more consistent.
A facilitator that I am wondering about is fostering relationships between patients. In the past I have seen the power of this peer support. On my HD unit, we had a waiting room. Before their runs, there was often quite a bit of discussion among patients in the waiting room. However, in my pre-dialysis kidney care clinic there is very little opportunity for patients to interact. I wonder if this is something we can work to develop?
What about in your clinics? Do you see some chances to lean on the facilitators and reduce barriers? I would love to hear your ideas!


