Speakers: Julie Scialla MD, Connie Weaver PhD RD
This is a summary of a presentation I attended at the National Kidney Foundation Spring Clinical Meeting in May 2024.
What is the history of cardiovascular disease (CVD) in CKD?
Early on it was recognized that in for adults living with CKD, traditional CV risk factors weren’t always present despite high rates of CVD. This led to the idea that a different mechanism might be a play. In early studies there was signals that phosphorus was stimulating vascular calcification.
What is FGF23?
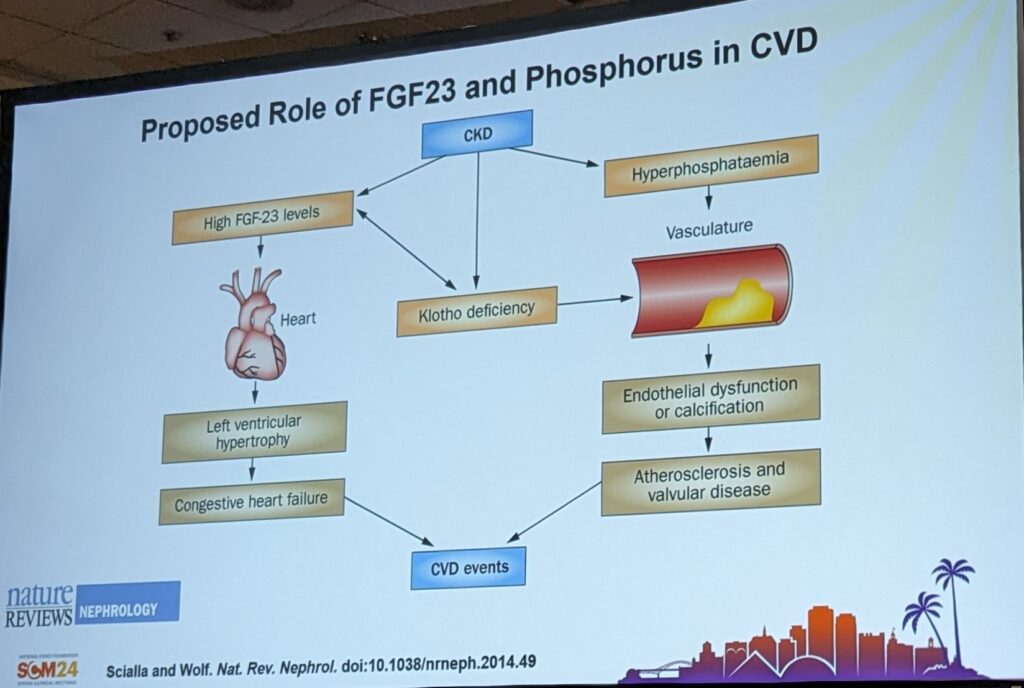
FGF23 stands for Fibroblast Growth Factor 23. FGF23 is a phosphorus-related hormone made in bone cells and high levels are strongly associated with mortality risk. This suggested that maybe it wasn’t the PO4 perse, but rather the FGF23 response to phosphate that may be contributing to calcification.
Is FGF23 the main contributor of calcification in CKD?
The CRIC study, started recruiting in 2003. They followed PO4 and FGF23 over years and looked at Coronary Artery Calcification. The strongest signal was that higher phosphate was associated with coronary artery calcification.
As FGF23 increased, atherosclerotic CVD and heart failure events increased. Suggesting a hypertrophic toxicity related to calcification, which is led by high phosphate levels. This all led to the paradigm that we should aggressively treat serum phosphorus levels.
Are phosphorus binders effective for adults living on dialysis?
Yes. Phosphate binders can lower serum phosphate by 1-2mg/dl. We do not know which binder is better.
Tenapanor is the newest phosphorus lowering medications, though it isn’t a binder perse. It works by lowering phosphorus absorption in the GI tract. Tenapanor can be combined with traditional binders or used alone (see my other post here for more info about Tenapanor).
Are phosphorus binders effective for pre-dialysis CKD?
No. In two studies, there were only small reductions in serum phosphorus levels with lanthanum vs placebo in this population. At this point, there are no FDA approved phosphorus binders in the pre-dialysis patient population.
But what does effective really mean?
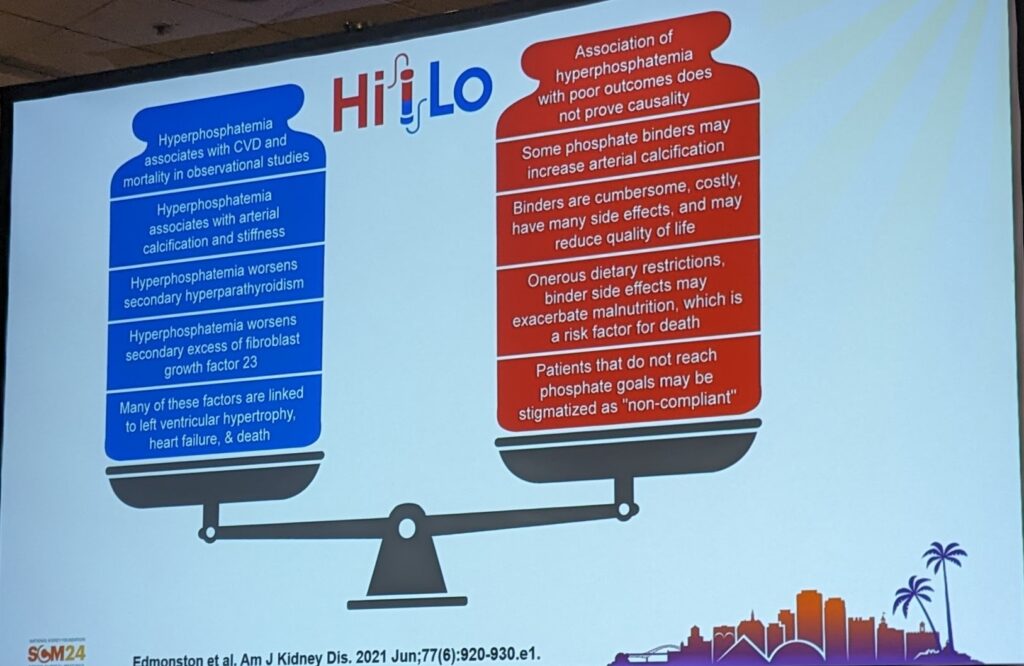
While it is well documented that phosphorus binders effectively lower phosphorus levels, clear mortality and reduced incidence of cardiovascular events haven’t been clearly shown with binder therapy. And this is the key point! We don’t REALLY care about serum phosphorus levels, what health care providers and patients actually want is to live longer, healthier, high quality lives.
So how do phosphorus binders improve outcomes that we actually care about?
A 2007 trial reported no improvements in all-cause mortality or CV mortality when sevelamer and calcium was compared. A problem with this study was that there were many drop-outs.
The Landmark trial compared lanthanum vs calcium based binders. The main outcome was mortality and CV events. Calcium and lanthanum results were very overlapping, with potentially small advantage to calcium over lanthanum.
Are there any studies underway to help use better understand how lower phosphorus levels is associated with outcomes?
- HiLo Pragmatic Trial of Phosphate Targets in the US on HD – this trial was recently stopped due to inadequate enrolment.
- PHOSPHATE Pragmatic Trial of Phosphate Targets in Australia (and Canada too!) – main outcomes are CVD mortality and events. We can expect results of this study in 2027/2028.
Are there trials with other binders that have been done?
Lanthanum vs Velphoro was compared with the outcome of coronary artery calcification (CAC) scores. Neither binder showed much difference, though there was potentially slight slowing of CAC with strict phosphorus control.
How does this data impact our current practice guidelines?
This has led to all of our guidelines being suggestions – based on basic science and observational studies as opposed to high quality clinical trials.
There is inadequate evidence that PO4 binders improve phosphorus levels in pre-dialysis CKD. Only observational studies suggest improved PO4 will improve outcomes for patients.
Calcium Intake Recommendations in CKD
Speaker: Connie Weaver PhD
Objectives:
- Review calcium metabolism and interactions with other nutrients
- Compared dietary sources of calcium
- Consider special issues of calcium in CKD
Recent European Recommendations suggested 800-1000mg total daily calcium for the CKD population. I reviewed these guidelines in a previous post, available here.
What nutrients are important for bone health?
Bone central nutrients include:
- Calcium
- Vitamin D
- Magnesium
- Phosphorus
- Potassium
- Protein
In the general population, most people do not get adequate amounts of bone-central nutrients.
If you get adequate phosphorus and calcium, then you will absorb about 80% of the phosphorus and 30% of the calcium. In the kidney, normally calcium and phosphorus is excreted if there is any excess.
Why does CKD impact bone homeostasis?
As PO4 retention increases there is a decrease in Vitamin D levels (1,25D) and increases in parathyroid hormone (PTH). Hyperphosphatemia is associated with soft tissue calcification, but what happens to the calcium?
Calcium storage in bone is a functional reserve and this is important for reducing fracture risk. Because calcium is lost, we have an obligation to obtain calcium from the diet to stay in calcium balance.
What factors impact calcium absorption?
In healthy individuals’ factors that affect calcium absorption include:
- As you eat more calcium, more calcium is absorbed, though the efficiency decreases.
- Calcium deficiency can slightly increase absorption but this adaption is relatively small. Calcium is absorbed via transcellular and paracellular pathways (just like phosphorus). Paracellular is linear while transcellular can saturate out.
- Lifestage – adolescents had better absorption than adults, absorption reduced with age.
- Source: dairy products contain a good combination of the bone-important nutrients (though this is challenging in the CKD population because dairy is also high in PO4 and K). They are higher in bioavailability for calcium than other foods, for example spinach or foods with oxalates or phytates
- Diet factors: sodium reduces calcium absorption, fibre increases absorption
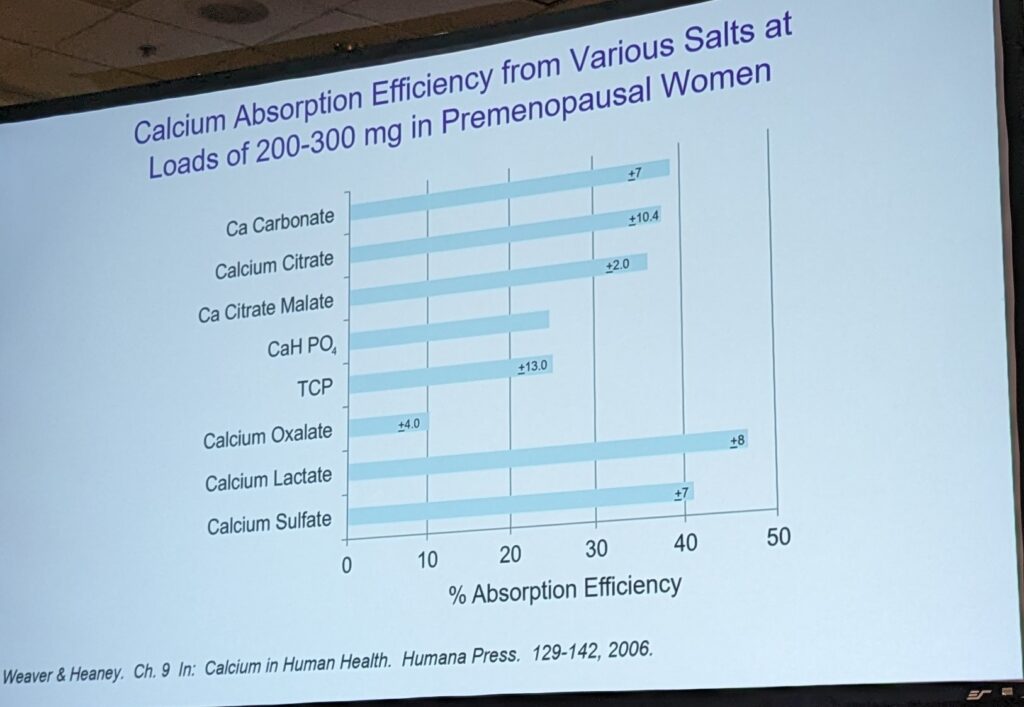
What about calcium supplements?
Calcium carbonate has the highest percentage of calcium and most calcium salts have fairly similar absorbability. Ca-carbonate is also the most affordable supplement. Calcium citrate has previously been reported to be better absorbed. However the isotopic tracers have suggested that infact their absorption is the same.
What studies have investigated calcium balance in CKD?
The use of calcium carbonate as a phosphorus binder resulted in increased fecal calcium excretion and lead to a positive calcium balance. This could be problematic. In healthy adults, the calcium balance wouldn’t become positive.
In this same study, the calcium based binder didn’t improve phosphorus balance. Calcium kinetic tracers demonstrated significant increases in balance, which could increase the risk of calcification of the soft tissues.


One thought on “Updates in Calcium and Phosphorus Metabolism”