This is a summary of a presentation I watched at the National Kidney Foundation Spring Clinical Meeting.
Speakers: Wesley Dutton MD, Desiree de Waal RD
Objectives:
- Goals of treatment and indications for anti-obesity medications (AOMs)
- Review approved medications and examine special considers for CKD
- Examine the second generation of anti-obesity medications
What is obesity?
A complex, multifactorial chronic disease of excessive or abnormally accumulated body fat mase. While it is recognized that BMI can be good for screening, it shouldn’t be used alone as a diagnostic tool.
What is causing obesity?
Environment and genetic factors. Environmental factors do not include choice or lack of will power. There is genetic susceptibility and environment risk factors similar to diabetes.
What is cardiovascular kidney metabolic syndrome?
The cardiovascular kidney metabolic syndrome describes a cycle of events that increase the risk of negative outcomes for our patients.
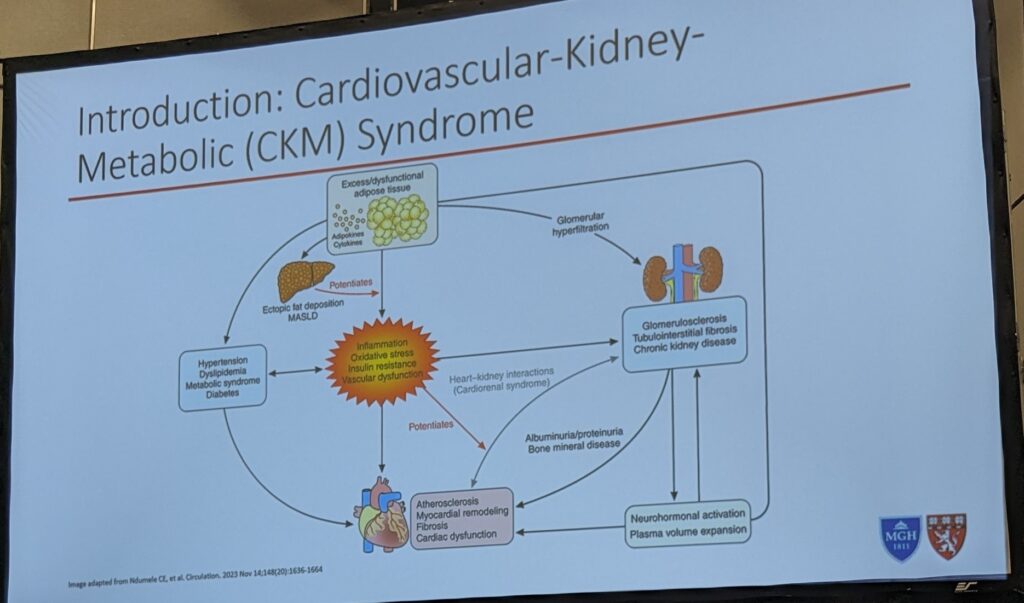
What is the link between obesity and CKD?
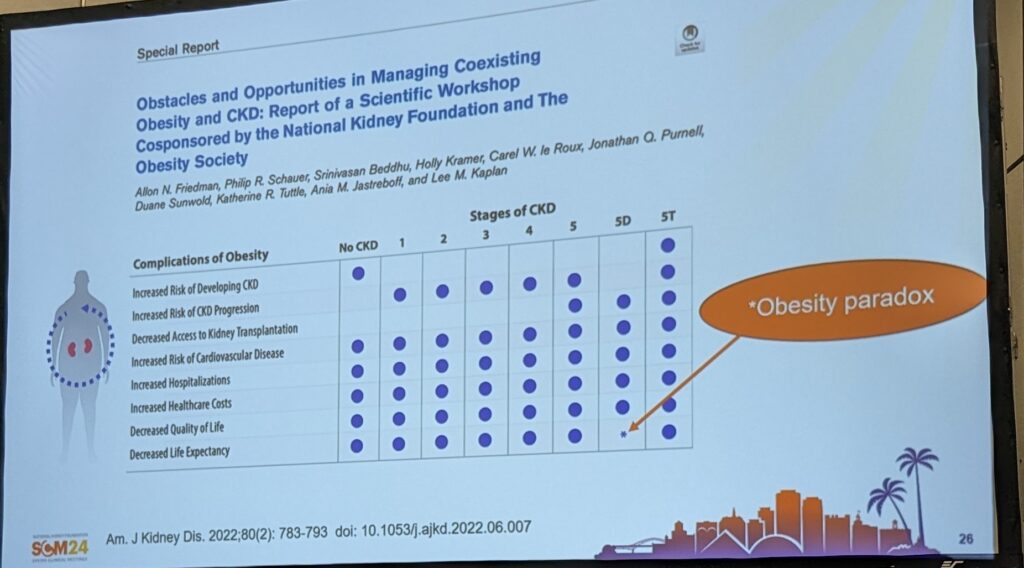
49% of people with CKD have obesity. Obesity can have hemodynamic and neuro-endocrine effects which can increase the risk of developing CKD. There also anatomic effects including fat compression of the kidney or ectopic lipid accumulation increasing the risk of CKD.
Obesity can also impact the ability to deliver CKD therapy including making vascular access harder, increasing the risk of PD complications and be a barrier to referral for transplant.
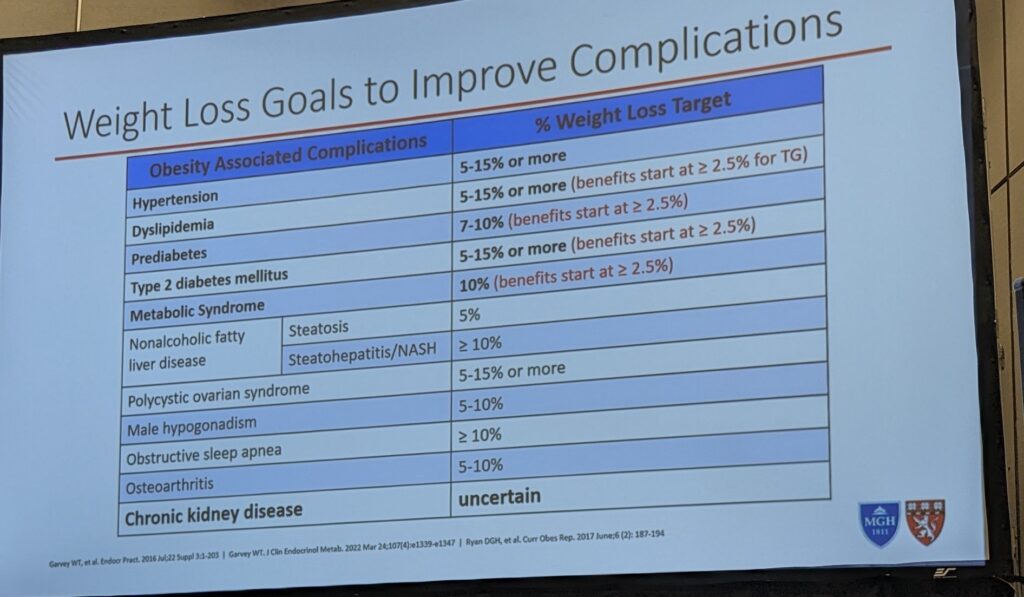
What are the goals of treatment for obesity?
The goal is to limit the health burden by reducing complications – HTN, T2DM, CKD and Obesity. The target is % weight loss to guide the prevention of complications.
Many benefits start at 5% weight loss, but we don’t know what % to target for CKD.
What are our treatment strategies?
- Lifestyle
- Medications – indicated if BMI over 27 with complications or BMI over 30.
- Use medications as an adjunct to lifestyle therapies. Anticipate needing to use the medications long term and titrate to the maximum tolerated dose.
- Surgery
- Or a combination of surgery and medications
What do the guidelines tell us?
The KDIGO 2024 guidelines recommend treating people with CKD with a comprehensive treatment strategy to reduce risk of progression. The guidelines state we should encourage people with CKD to achieve an optimal BMI and physicians should consider advising people with obesity to lose weight.
How to select a medication for weight loss?
- Efficacy
- Additional benefits (e.g. blood glucose lowering if a patient also has diabetes)
- Contra-indications and side effects
- Patient preference
- What is accessible to the patient (e.g. insurance coverage, drug availability)
What medications are used (in the USA) for weight loss?
| Medication (year of release) | Efficacy (% weight loss) | Side effects specific to CKD | Contraindications | Prescribing |
| Orlistat (1999) | 3% | Decreased absorption of fat soluble vitamins Altered medication absorption | Increased risk of kidney stones | Renal dose adjustment not needed |
| Phentermine (1950s) | 7-9% | Tachycardia and elevated BP | History of CVD or uncontrolled HTN | Requires renal dose adjustments. eGFR 15-29 max 15mg per day. Avoid eGFR under 15. |
| Phentermine/Topiramate (2012) | 9-11% | Tachycardia and elevated BP | Same as phentermine + metabolic acidosis, kidney stones, hypokalemia and decreased in renal function | Avoid use if on dialysis. If CrCl under 50 to avoid. |
| Naltrexone/Bupropion | 6-9% | Elevated BP and tachycardia | Uncontrolled HTN | Mod to severe renal impairment, avoid use on dialysis |
| Liraglutide 3.0mg (Saxenda) (2010 for DM, in 2014 for Obesity) | 6-8% | AKI related to volume depletion r/t GI side effects | Hx of thyroid cancer | No dose adjustment for renal impairment; Start low and slowly titrate to prevent GI side effects |
| Second Generation Medications | ||||
| Semaglutide (also reduces BG and CVD risk) | 15-16%; 51-64% had more than 15% weight loss | AKI related to volume depletion | Same as liraglutide | Same as liraglutide |
| Tirzepatide | 21-24%; 71% had more than 15% weight loss | AKI related to volume depletion | Same as liraglutide | Same as liraglutide, Can increase every 4 weeks as needed |
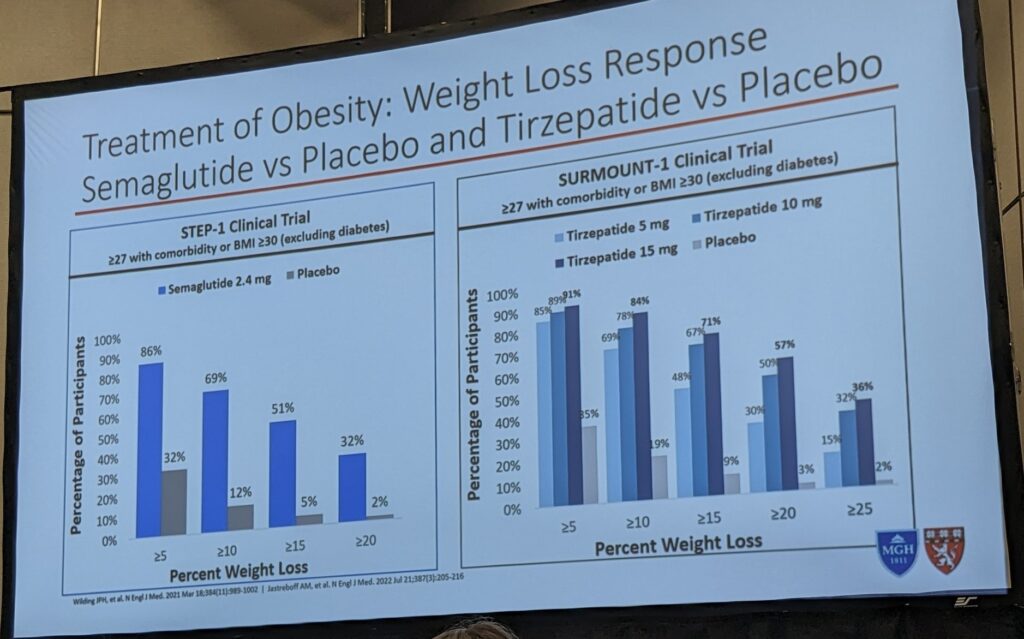
What are the second-generation medications?
Medication that promotes at least 10% weight loss and the ability to produce at least a 15% weight loss in more than 50% of patients when combined with lifestyle interventions.
How much weight loss is anticipated with the second generation medications?
What are the systemic effects of GLP-1?
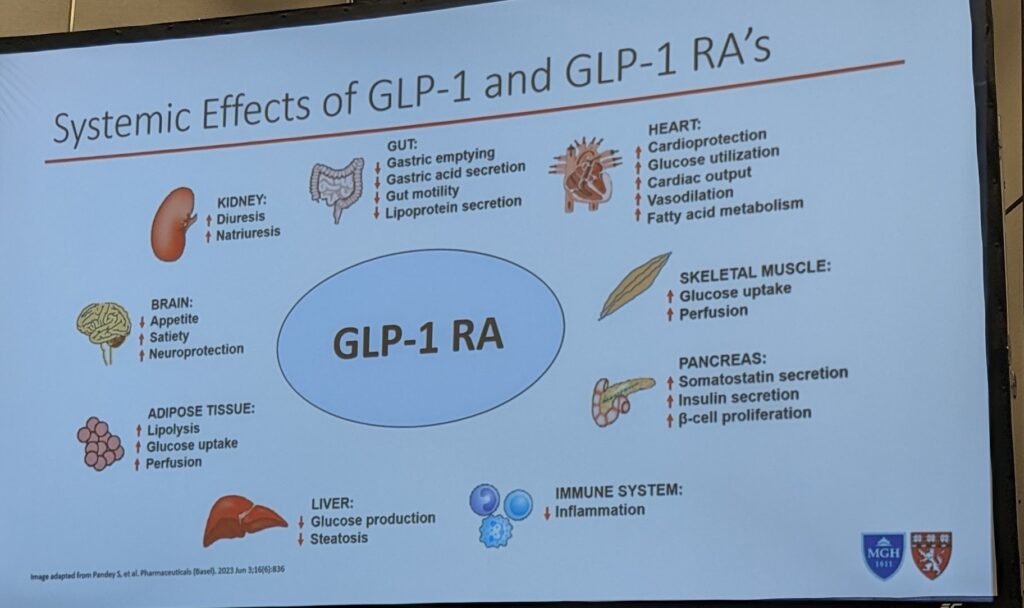
What about secondary outcomes of the GLP1s?
- Improved BP
- Improved lipid profiles
- Improved glucose control
Do GLP1s reduce the risk of CVD and CKD?
Yes! GLP1s are associated with risk reduction in both CVD and CKD outcomes.
The SELECT trial investigated this in patients without DM. Over 17000 people participated. The Hazard ratio was 0.8 – which suggests a 28% reduction in cardiovascular risk. This benefit was also seen in the group of participants who had an eGFR under 60.
The hazard ratio for renal death or starting dialysis was 0.78. This suggests a reduced risk of nephro-specific outcomes. A meta-analysis has also confirmed reduced risks of CVD and worsening nephropathy for GLP1s used in people with DM.
The FLOW trial evaluated the progression of CKD among adults living with CKD and DM. There were statistically significant decreases in kidney disease progression, CVD and kidney death. The trial was stopped early due to demonstrated efficacy.
Tirzepatide is currently being investigated for it’s effects on CVD and CKD outcomes.
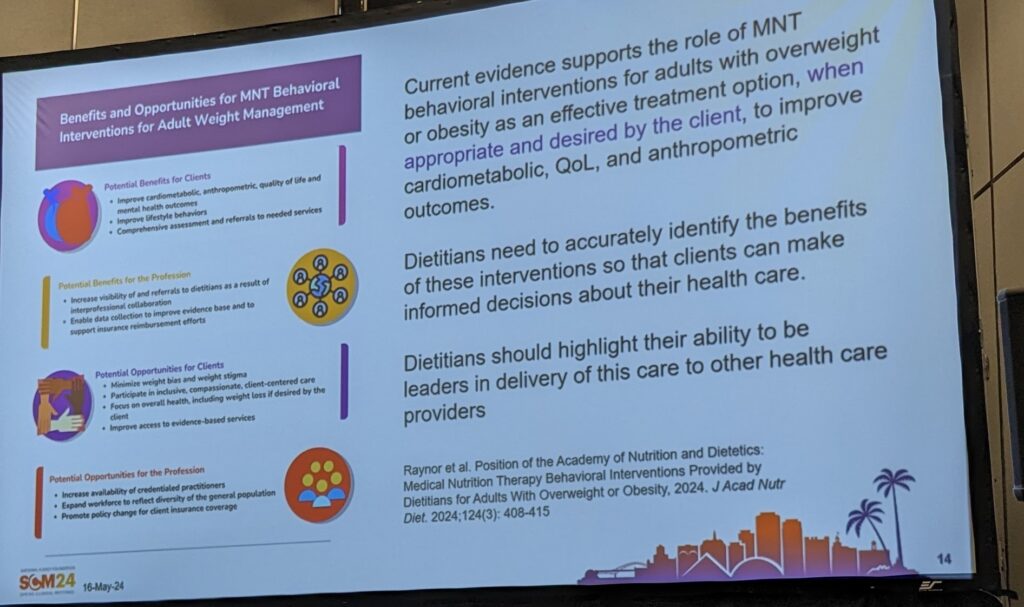
What is weight stigma?
Weight stigma has compromised many aspects of obesity care. Weight stigma is negative beliefs or attitudes about a person’s weight. It can disempower people to access care.
Fatphobia in healthcare is the assumption that excess fatness means poor health poor food choices and limited exercise, laziness, unattractiveness and poor hygiene.
What is a weight neutral approach?
Recognizing that one’s health is more than a number on the scale. Everyone has the potential for well being independent of their weight. It recognizes the role of stigma in accessing health and includes social determinants of health.
Weight centric approach – aims for a certain body weight, good and bad type thinking and focus on calories and portion sizes.
Weight natural is the pursuit of self care instead of weight loss. It acknowledges that bodies will seek natural weight when natural responses and cues are listened to. The goal is use an all food fits approach and to determine the quality and quantity of food using physical cues. There is a focus on enjoyment in movement.
There is a wild-held assumption is that weight loss is attainable for the majority of people if they try hard enough, except evidence suggests this isn’t the case. In fact, more than 95% of people who attempt weight loss will fail. No diet or exercise therapy plans have ever been able to demonstrate maintained weight loss over several years.
What is the best diet for weight loss?
There is no proven specific diet that is durable and sustainable for weight loss.
What are the risks associated with weight loss interventions?
Greater BMI variability is linked to an increase risk of all-cause mortality and a 20% increase in MI.
What counseling tools work?
There is no one specific tools that will work for each patient. Different strategies work for different patients.
- 6 stages of change
- Motivational Interviewing
- Cognitive Behaviour therapy
- Solution focused therapy
- Intuitive Eating
- Influencer Model
Do all patients have the same risk of developing obesity?
People of colour have higher rates of obesity, DM and CVD and are under-represented in health care. We must consider clients’ diversity and lifestyles, experiences and perspectives. Our goal should be to respect cultural differences and values of our patients.
How should we talk with our patients about weight loss?
- Avoid scare tactics
- We need to build trust with our patients so they feel comfortable telling us the truth
- There is so much information at us everywhere about diets and weight loss
What are the challenges for obesity management in CKD?
- Concern with the obesity paradox for those on dialysis (those with large bodies appear to live longers)
- Hard to preserve muscle mass (concern with sarcopenic obesity)
- Limited resources for intensive lifestyle interventions
- Limited knowledge and experience with medications
- Concern with bariatric surgery in the co-morbid population.
What are the diet recommendations while on GLP1?
- Small, frequent meals can help reduce GI side effects, aiming for eating at minimum every 4-5 hours during waking hours. Nausea can be worse if there are longer periods of times without food.
- May require higher nutritional density foods (e.g. supplements) if unable to meet nutritional requirements



One thought on “Nourishing the path to wellness: exploring the role of pharmacy and nutrition in managing obesity in CKD”