This is a summary of a presentation I watched at the National Kidney Foundation Spring Clinical Meeting.
Speakers: Connie M Rhee MD, David St-Jules RD PhD, Lisa Koester NP
How does phosphorus management contribute to pill burden?
Median pill burden in ESRD is ~19 pills per day with about 25% being phosphorus binders. Higher pill burden is associated with reduced quality of life.
What are the patient perspectives on phosphorus management?
A study investigating patient perspectives on phosphorus management, reported that patients:
- Felt they weren’t explained the rationale for controlling phosphorus
- Experienced frustration around lack of phosphorus labeling on food products
- Found social and family gathering are more challenging
- Worried if they missed their binders
- Found binders harder to take when they were eating outside the house
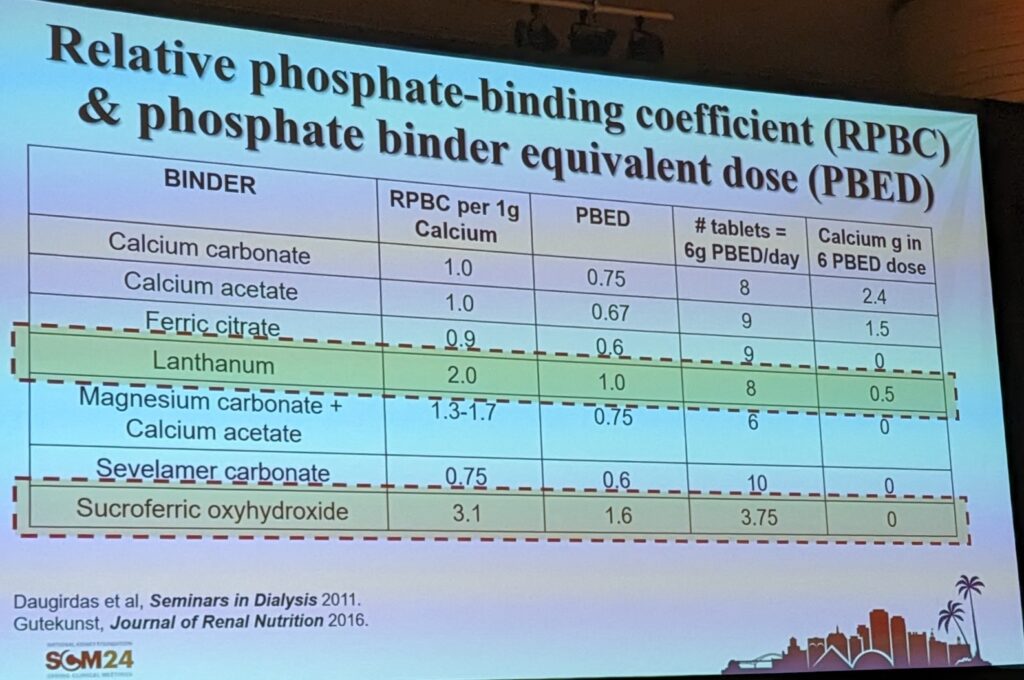
What is the phosphorus binding capacity of different binders?
Different binders have different binding capacity. Don’t forget the calcimetics – which can also help reduce serum phosphorus levels. Typically binders are still required for those on dialysis as there is limited phosphorus removal from dialysis.
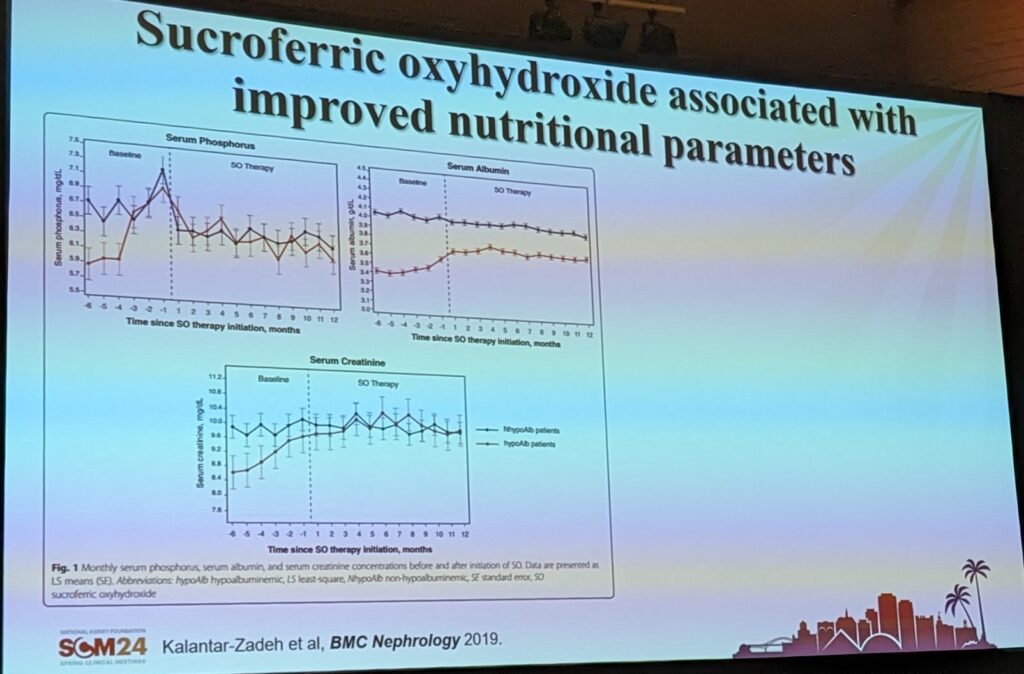
Have binders been associated with improvements in nutritional status?
Data has suggested that binders can be used to help support nutritional status. My two cents: Intuitively this makes sense given the potential that binders could have in liberalizing dietary phosphorus restriction.
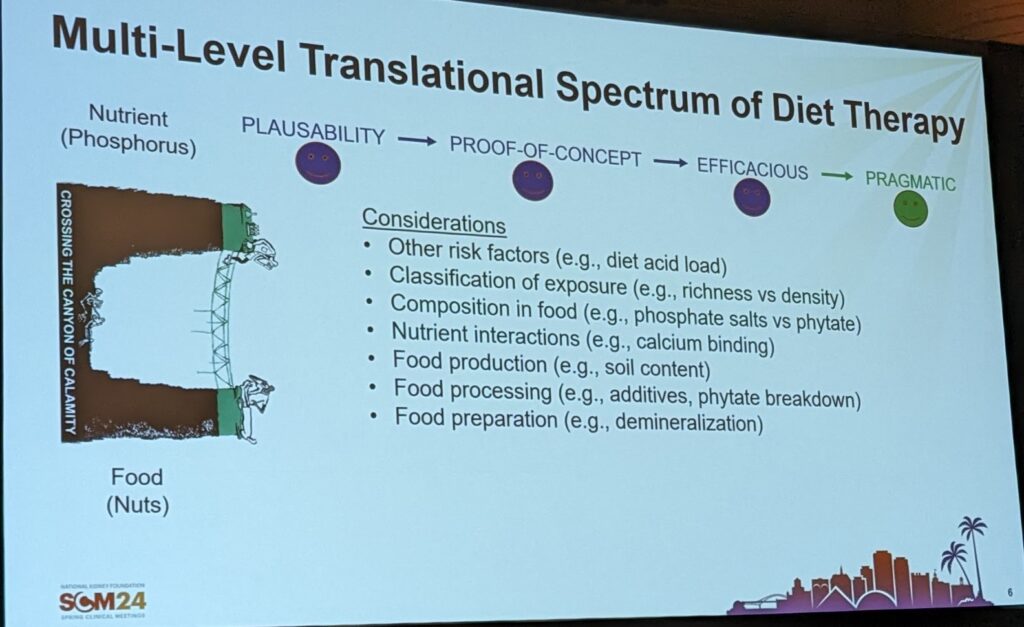
How is nutrition research translated from evidence to food?
Mechanism/effect observations demonstrate that a concept could be plausible. This is followed by controlled feeding or supplementation trials in animals which can confirm concept. The next step is behaviour interventions trials to test efficacy with a final step of pragmatic trials where we test an intervention in free-living humans.
However, in feeding studies if the focus is on single food, this can reduce the real-life applicability. This is because people tend to eat foods in groups (e.g. cereal with milk), so studying individual foods may also have less fidelity in free-living humans.
What research methods can be used to understand if someone should or shouldn’t eat something? An example with whole grains
Guidelines tend to focus primarily nutrients – e.g. limit or adjust phosphorus. They don’t specify anything about what foods to include. A survey of dietitians suggested about half of dietitians sometimes restrict whole grains. Studies have found that patient handouts primarily restrict whole grains and recommend refined grains.
The two approaches to study this are:
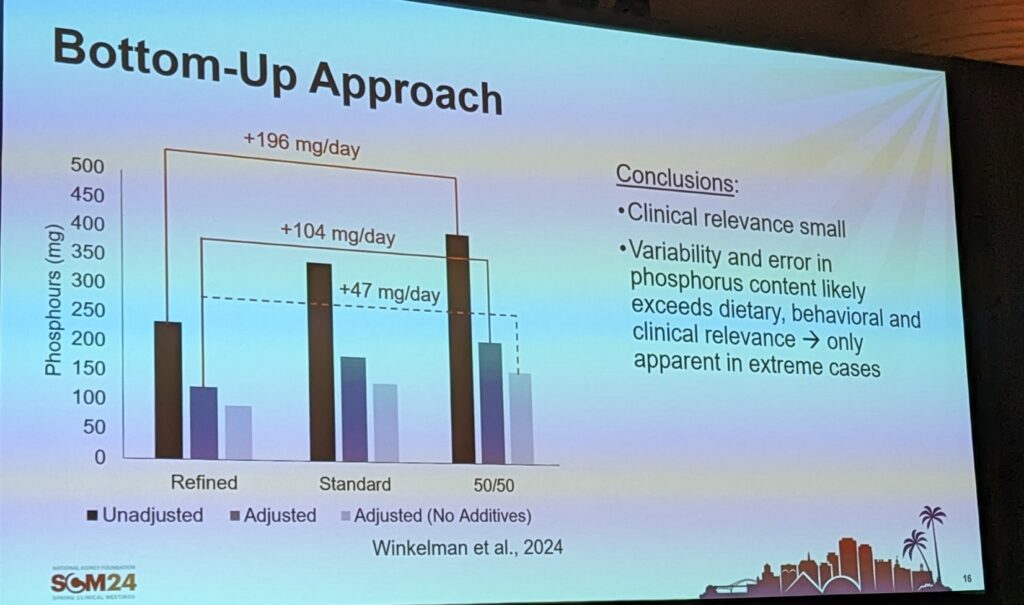
- Bottom-Up Approach – assess phosphorus exposure from refined and whole grain diets
- Modeling studies do not suggest that whole grains will add significant amounts of phosphorus (+47mg per day) (see the slide above)
- Top-Down Approach – evaluate the association of reported whole grain intakes and clinical outcomes
- Observational studies have reported that serum phosphorus levels are lower when people consumed more whole grains. And whole grain density suggests that mortality is lower when people consume more whole grains per 1000kcal.
To date, these studies do not support that whole grains are problematic for CKD, however, much more research is still needed.
What does restriction of diet really mean?
Restriction of diet means that inability to participate fully in the social and joyful aspects of eating.