When I think of malnutrition, a condition characterized by inadequate intake and reduced nutritional stores, I worry about so many components for my patients.
And while I think dietitians are very good at thinking about malnutrition, sometimes we aren’t always the best at using validated tools to assess it, track it and most importantly communicate it to our health care colleagues.
Medical people love numbers – that’s why we do so much lab work. So I think, as dietitians it is very important that we do our best to put a number or a letter or grade to someone’s nutrition status. But what tools should we use?
Today’s post, I am looking at the Chapter 5 of the 2024 KDIGO Guidelines.
Practice Point 5.2.3.2: Screen people with CKD G4-G5, aged >65 or poor growth (pediatrics), or symptoms such as involuntary weight loss, frailty or poor appetite twice annual for malnutrition using a validated assessment tool.
How common is malnutrition?
KDIGO highlights that as many as 11-50% of adults with CKD have malnutrition. Risk factors can include:
- Increasing age
- Female gender
- Psychiatric disease
- Worsening kidney function
- Co-morbid conditions, including diabetes, autoimmune diseases, CVD
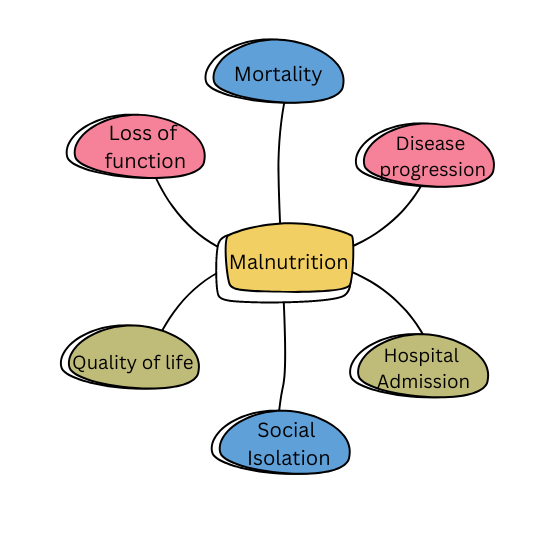
What’s wrong with malnutrition?
Malnutrition is associated with:
- Increased morbidity (disease progression/illness)
- Increased mortality (death)
- Loss of muscle mass
- Inflammation
- Worse outcomes post kidney transplant
What causes malnutrition?
In CKD, both the uremic toxins, which reduce appetite, and inflammation are thought to cause malnutrition.
How should malnutrition be assessed?
According to KDIGO 2024 three tools are recommended to assess for malnutrition in the CKD population:
- 7-point SGA (Subjective Global Assessment)
- MIS (Malnutrition-Inflammation Score)
- MNA (Mini-nutrition assessment)
I attended a great session at the National Kidney Foundation Spring Clinical Meeting that covers both the 7-point SGA and the MIS.
Take Aways
I will admit that I wasn’t always so keen on using a validated tool to assess malnutrition. I remember feeling like it was just another thing my manager was asking me to do. So what changed that for me?
- First, in order for us to do meaningful, clinical based nutrition research in our patient population, we need to use validated tools so that we properly characterize the populations we see and how our interventions make a difference
- Second, doctors and nurses and many of our other health provider colleagues like numbers. When I tell my colleague that this person scored a 2 out of 7 on a malnutrition tool and has severe malnutrition, I find much better uptake of my recommendations.
- Finally, I truly believe that using these tools means I am conducting better, more comprehensive assessments and gives a greater sense of purpose and joy in my practice.
In my current role I use the 7-point SGA. In a previous job (not in renal actually) I used the MNA. In both cases, I found these tools quick and easy to use in my clinical practice.
What tools are you using in your practice? If you are using them, what do you like? If you aren’t using them, what’s your biggest barrier? I would love to know!