This is a summary of a presentation I watched at the National Kidney Foundation Spring Clinical Meeting.
Speakers: Kam Kalantar-Zadeh MD, Kristin Larson NP, Wei Ling Lau MD
Objectives:
- Describe risk factors and clinical outcomes associated with recurrent hyperkalemia in those with and without CKD
- Discuss the importance of RAASi for cardiorenal protection
- Describe the role of novel potassium binders
What is hyperkalemia?
This definition may be discipline specific, for example nephrologists tend to accept a higher value than family medicine or cardiology.
- Mild is greater than 5.0mmol/L
- Moderate is greater than 5.5mmol/L
- Severe is greater than 6.0mmol/L – thought the speaker highlights that she is still not really getting excited at this value.
She highlighted the importance of considering if the potassium is acute or chronic and enforced the importance of considering what is normal for your patient. An article was written that reviewed the psychological burden of hyperkalemia. It was a NKF study in 2017.
Risk factors for hyperkalemia
- Cellular trauma including crush injuries, GI bleed, rhabdo and tumor lysis
- Metabolic acidosis
- Hyperglycemia
- Hypoaldosterone
- Medications
- NSAIDs – don’t cause it but tend to be part of the clinical picture
- RAASi
- Salt Substitutes (KCl)
- Natural Health Products/Supplements
- AKI
- Pseudohyperkalemia – a Canadian article reported that this could be as high as 33% of all samples. The number one cause was fist clenching during the lab draw. In addition is the collection technique, keeping samples on ice or delayed centrifugation. Unfortunately, the only way to identify a hemolyzed sample is to redraw it.
Is hyperkalemia an issue for CKD?
It can be attributed to 2-5% of deaths in Stage 5 CKD and the cause of 24% ER visits in the HD population.
This slide showed a good summary of the symptoms/clinical manifestations of hyperkalemia:
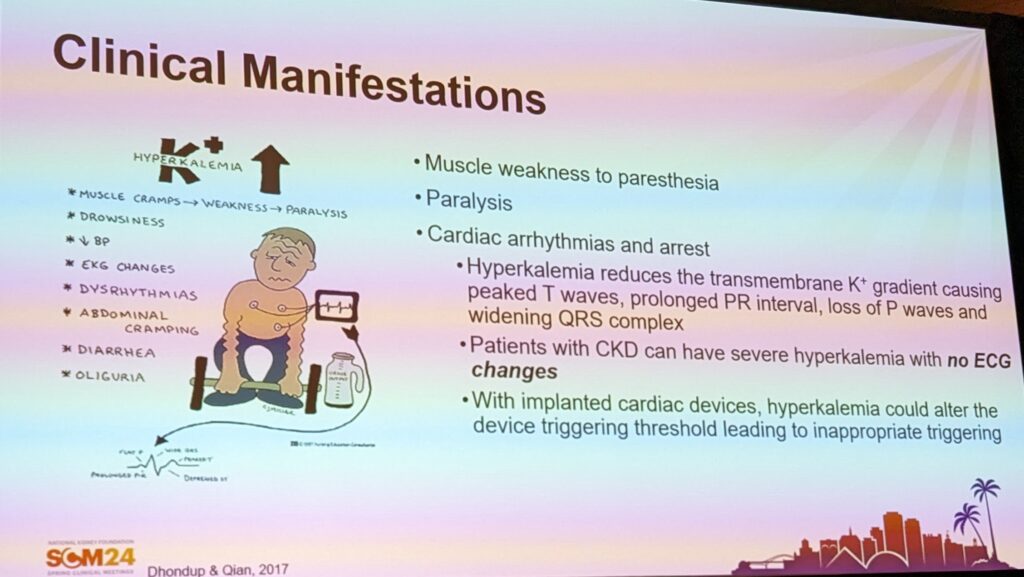
Those with battery operated devices in their body may be at higher risk of experiencing ECG changes from hyperkalemia.
Considerations of hyperkalemia management from a dietitian
- Label reading
- Life must be lived – diet coaching without shame, finding balance in foods that are chosen
- Anticipate high potassium times (holidays and garden seasons)
- Moving away from a traditional renal diet to maintaining potassium in health range for that person
- Involve social work for resources to obtain healthy foods
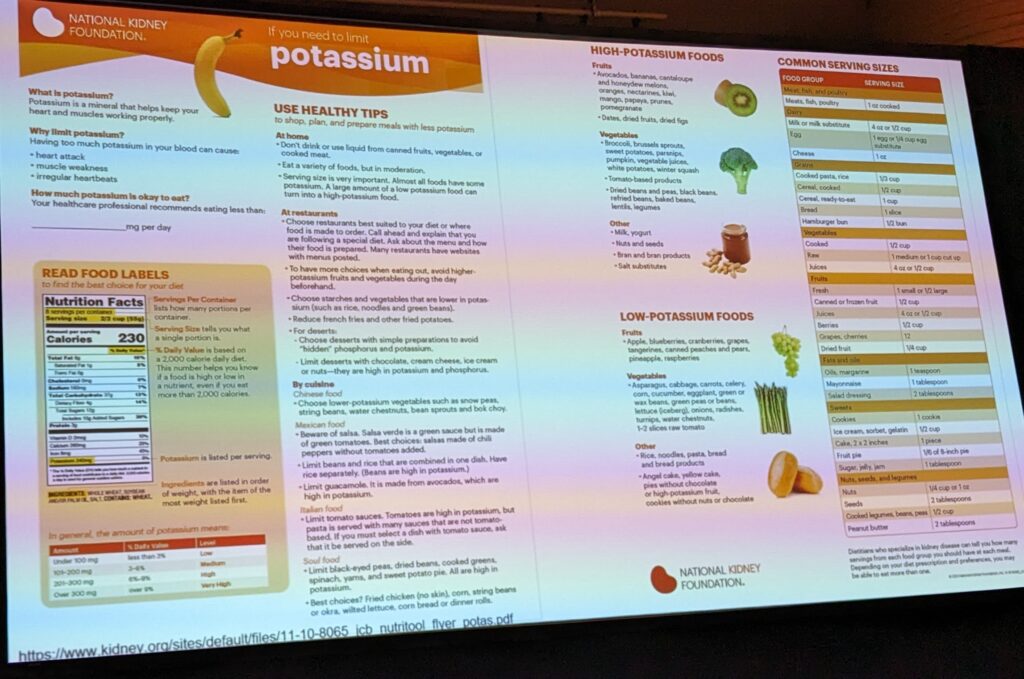
The NP recommended making food swaps: instead of bananas or oranges, choose canned peaches or instead of potato or tomato have green beans or carrots
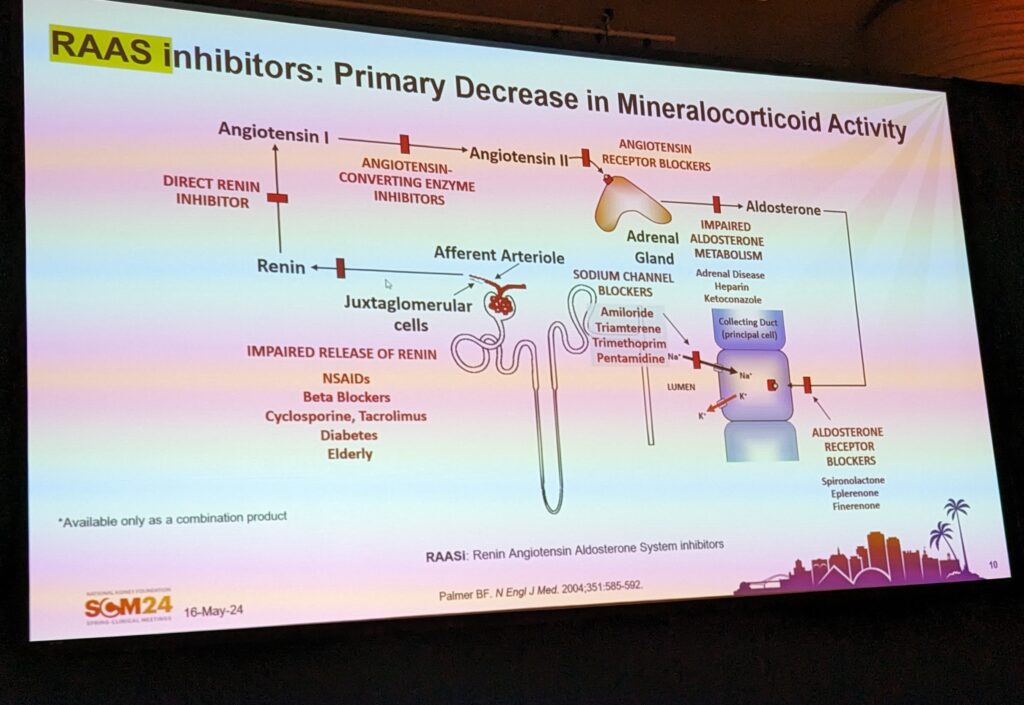
A Review of the RAASi system
Evolution has really focused on how to increase blood pressure to ensure we are able to stand up and move around. The kidneys are also hungry for adequate blood pressure for adequate blood profusion. It does this by conserving sodium and excreting potassium.
However, in 2024 we no longer need high blood pressure, we need low blood pressure. There are many medications that will impact the RAASi system. The main outcome of RAASi system disruption is potassium retention.
Why is RAASi important?
RAASi is the guideline directed medical therapies for heart failure with reduced ejection fraction. Two of the four pillars of the CKD in DM are also RAASi.
RAASi promotes kidney and life saving benefits in patients with CKD, Heart Failure, DM and Hypertension.
Dr. Kam Kalantar-Zadeh
Why is RAASi associated with hyperkalemia?
Reduced secretion of aldosterone and increased resistance to aldosterone. This is particularly challenging because most disease states where RAASi is indicated are at higher risk of hyperkalemia already.
RAASi-associated hyperkalemia is related to an increased risk of CV events, hospitalizations and death. YET, discontinuation of RAASi for patients with CKD or heart failure is also associated with increased risk for CV events, hospitalizations and death.
What happens when someone on RAASi develops hyperkalemia?
Data shows that more heart failure patients are admitted to hospital with hyperkalemia since the use of spironolactone was started for these patients. Hyperkalemia is the leading cause of RAASi discontinuation. It is also the number one reason that these medications aren’t started. But those patients who don’t receive the max dose or who have it stopped – are those who have the highest mortality rates.
What about newer medications are they any better?
Unfortunately, no. Newer generation of MRA – finerenone, also improves outcome but they are also associated with increased serum potassium levels. The most common adverse events reported in the studies continues to be hyperkalemia.
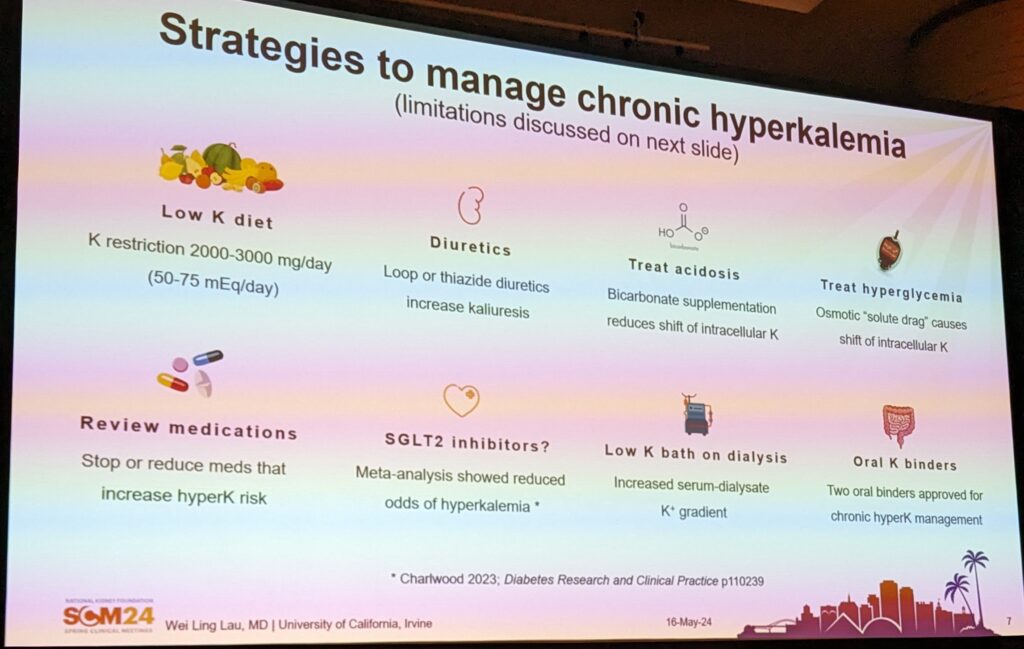
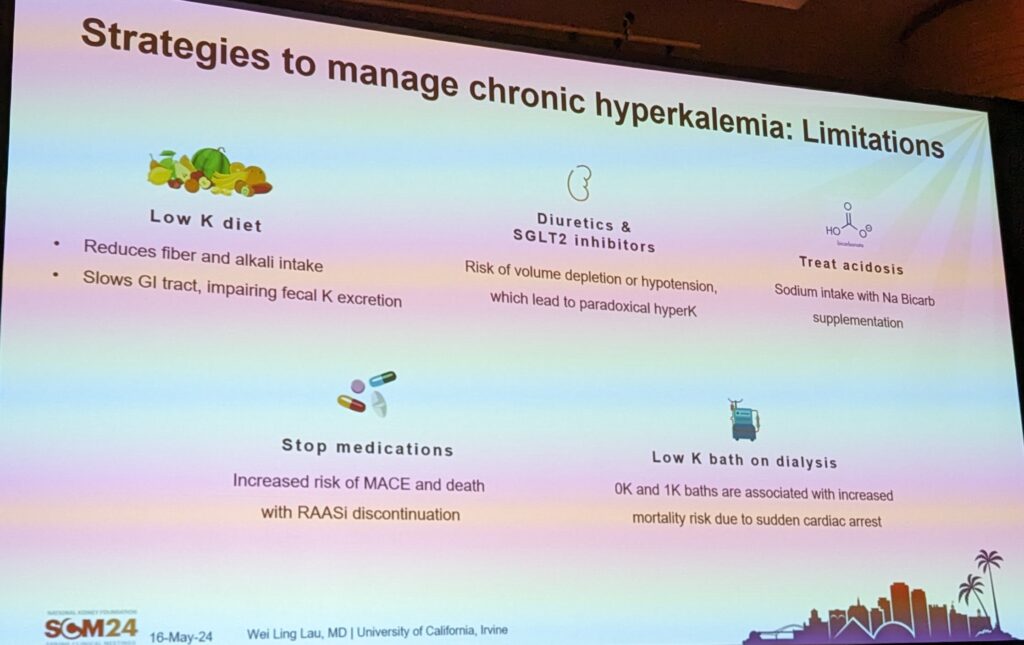
What strategies can be used to manage chronic hyperkalemia? And what are their limitations?
What oral potassium binders are available?
- Sodium polystyrene sodium (SPS) (1958) – has an increased risk of intestinal necrosis, though for every 5 million doses prescribed annually in the USA, there were only 58 events reported between 1948-2011. So this risk is very low. Does not appear to be associated with the sorbitol alone. SPS appears to be the offending agent.
- Patiromer (2015) – exchanges calcium for potassium, also binds magnesium – so need to watch for hypomagnesemia. Avoid sprinkling on hot food or taking with hot liquids. Avoid taking at the same time as other medications, specifically thyroid medications. Action tends to be in the large intestine.
- Sodium Zirconium Cyclosilicate (2018) – exchanges sodium for potassium. Action is in the small intestine. Interacts with out medications.
Patiromer interactions with ARBs, Beta-blockers, antibiotics, thyroid, metformin, Mycophenolate. OK to take with their phosphate binders.
Do potassium binders as adjunct therapy with RAASi prevent hyperkalemia?
Yes. In a study of CKD patients with DM, who started with a potassium above 5.0mmol/L. Patiromer dosed to achieve potassium values under 5.0mmol/L for 1 year reported that patients were able to maintain their RAASi doses. In another study, adding novel potassium binders enabled patients to continue or start RAASi therapy.
What are the risks of novel binders?
- Often GI related (constipation, diarrhea, abdo pain, flatulence)
- SZC has an increased risk of edema due to exchange of sodium for potassium.
What if they don’t like it?
OK to mix into juice or soft food such as applesauce, pudding or yogurt.