As a renal dietitian, when I think about hyperkalemia, I think about adults living with kidney disease, but of course hyperkalemia is common in other populations too. So today’s post focuses on hyperkalemia in adults living with heart failure (HF).
What are the risk factors for hyperkalemia among those with HF?
According to the article, specific risk factors for hyperkalemia are:
- HF severity
- Low hemoglobin
- Baseline high potassium
- Low kidney function
Is hyperkalemia associated with worse outcomes in this population?
Hyperkalemia has been associated with increased hospital admission, readmission and mortality. Furthermore, one study reported that correcting hyperkalemia reduced mortality risk. However, it is important to note that both of these these studies were retrospective so we can’t conclude that it was the hyperkalemia that caused the mortality. It is possible that was it something else that caused both the hyperkalemia and the death.
On the flip side, some studies have reported that hyperkalemia (potassium levels between 5.0-5.5mmol/L) were associated with decreased mortality risk.
One hypothesis for the HF population, is that hyperkalemia may be good or bad depending on the cause. For those with hyperkalemia related to drug therapy, hyperkalemia may be protective because this means the medications are working. While for those with hyperkalemia related to kidney function or critical illness, hyperkalemia tends to be associated with higher rates of arrhythmias and cardiac arrest.
What is the optimal range of potassium for people with HF?
According to this article, the ideal range is 4.0-4.9mmol/L, though values between 5.0-5.5mmol/L appear relatively safe.
That being said, the authors highlight that a 2017 study reviewing medical records of 911,698 people found that all-cause mortality rates per index potassium was consistently higher for those with HF than the healthy controls, people with CKD and people with DM. And based on this article, the ideal upper limit for potassium for people with HF was set at 4.8mmol/L.
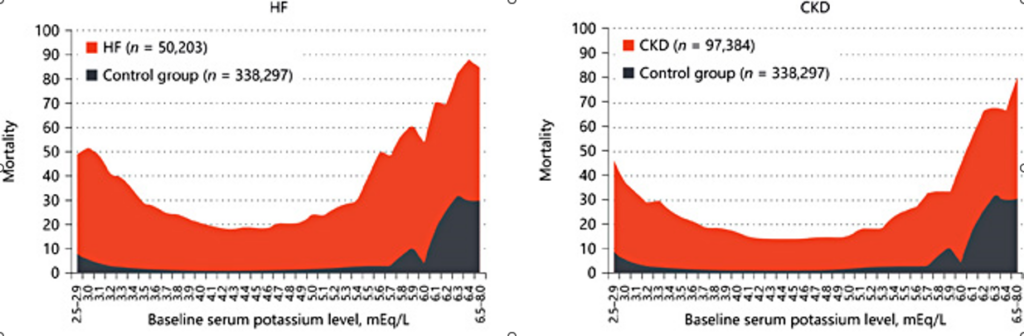
Figure 2 from the 2017 study is shown above. I liked this graphic and they way mortality rates were compared to healthy controls for both HF and CKD. What to notice from this figure is how much more RED is on the HF graph compared the blue and compared to the amount of RED on the CKD graph. A lot more!
How much do HF medications increase potassium by?
Both RAASi and MRAs have been reported to increase potassium levels from <2% to 5-10% depending on the patient. Patients with only hypertension tend to have smaller increases, while patients with kidney disease have the largest increases. MRAs (spironolactone and eplerenone) also tend to be more strongly associated with hyperkalemia because MRAs increase potassium absorption.
If hyperkalemia presents should medications be stopped or reduced?
Similar to CKD, in adults with HF, medications such as RAASi and MRA are associated with significant mortality benefit and the goal is to get people on these medications and at target doses. As such, that authors explicitly state:
Therefore, optimizing the therapeutic dosage of RAASi is encouraged, despite any difficulties in managing hyperkalemia.
Inability to get to target doses of these medications reduces the effectiveness. Additionally, evidence suggests that when these medications are stopped due to hyperkalemia, they are unlikely to be restarted.
How often should potassium levels be checked?
People living with HF and CKD, have potassium levels above 5.0mmol/L or who have renal stenosis, recommended monitoring depends on the medication.
For RAASi the recommended monitoring is:
- 1-2 weeks after starting
- Every 3-5 months
For MRAs the recommended monitoring is:
- 1 week after starting
- 4 weeks after starting
- Every 3 months
The authors recommend that medications be stopped or tapered if the potassium levels are above 5.5mmol/L, though attempts should be made to restart medications.
How should hyperkalemia be managed?
The final section of this article starts to discuss hyperkalemia management. Highlights that dietary counseling for potassium and looking at other medications (such as potassium supplements or NSAIDs) should be considered. The authors do not get into any dietary counseling specifics.
They also discuss pharmaceutical options for hyperkalemia management – specifically sodium polystyrene sulfonate (often known in clinical practice as Kayexalate). And the new medications Lokalma and Veltassa. Kayexalate comes with it’s own concerns, specifically the risk of hypernatremia, volume overload and GI complications. Lokalma and Veltassa are newer options and some studies have been conducted among those with HF.
Both agents have been studied among those with HF, but unfortunately these studies have been short and targeted at maintenance of normokalaemia vs emergency treatment of hyperkalemia.
In my practice, I find lack of coverage for these medications remains a significant barrier to their routine use.
Take Aways
- Adults living with HF are at high risk of hyperkalemia, largely related to guideline recommended medications which increase potassium absorption (MRAs) and decrease potassium excretion (RAASi)
- Managing hyperkalemia using diet or other medications is preferred to stopping guideline-recommended medications that are known to improve outcomes in this population
- Ideal serum potassium targets might be tighter for HF then other high risk groups, such as those with CKD or DM, because evidence suggests they have higher mortality rates from hyperkalemia
But as a dietitian, my question of but how low can dietary potassium intake go? And how can I ensure my patients aren’t becoming malnourished along the way? Are not questions answered by the article. For help with hyperkalemia management – head over to my subscribers only page and pick up one of my hyperkalemia assessment cheat sheets.
Though I can promise there will be more to come on hyperkalemia and HF.