Given that constipation is known to contribute to hyperkalemia risk and many ostomies are associated with increased fecal volume, the most well-known impact is hypokalemia.
However, did you know that not all ostomies are associated with hypokalemia? And in fact, can be associated with hyperkalemia? I have observed this a number of times in my clinical practice. And that’s why I mention the impact of ostomies on my hyperkalemia assessment guide.
So let’s dig into what the literature says about the phenomenon.
A shout out to my good friend who asked me to write this post. She also sent me much of the literature I will be talking about today.
What does the literature say?
There are two published case reports describing this phenomenon.
The first case describes a 56 year old women on maintenance dialysis who had a temporary ileostomy created. Her ileostomy was associated with a 1.1mmol/L on average increase in her serum potassium levels, ranging from 6.1-8.3mmol/L. The authors report that they tried low potassium diets and potassium-binding medications. In the end, her ileostomy was reversed, and her potassium values returned to baseline.
The concentration of potassium in the tool was tested while she had her ostomy and after it was reversed. The potassium concentration in the stool after reversal more than doubled! This led the authors to conclude that hyperkalemia was directly related to her ileostomy. Specifically related to reduced fecal potassium excretion.
The second case describes a woman in her 60s, also on maintenance dialysis, who developed hyperkalemia post ileostomy creation. Her pre-dialysis serum potassium values went into the 6.0s. She did not have a history of hyperkalemia prior to her ileostomy. To rule out a concern with inadequate potassium removal during dialysis, the authors of this study checked her potassium post-HD. They reported a post-run potassium value of 3.5mEq/L. The person was also started on a potassium-binding medication with minimal effect.
The authors of the second paper concluded that her hyperkalemia was related to reduced colonic excretion of potassium.
How can this be explained?
In the nutrition management guidelines for patients with a short bowel, there is a small section that discusses sodium, fluids and potassium.
In this paper, the authors highlight that patients with jejunostomies tend to have large output from their stoma. And that the output can be even higher after eating or drinking. The output from ostomies and jejunostomies contains very little potassium, with the authors reporting only 15mmol/L. The authors state that there will only be potassium losses if more than 50cm of the jejunum is intact.
For adults with normal kidney function, potassium balance is maintained through additional potassium excretion in the urine. However, for those without normal kidney function, this compensatory mechanism could be compromised and result in adequate potassium excretion, leading to hyperkalemia.
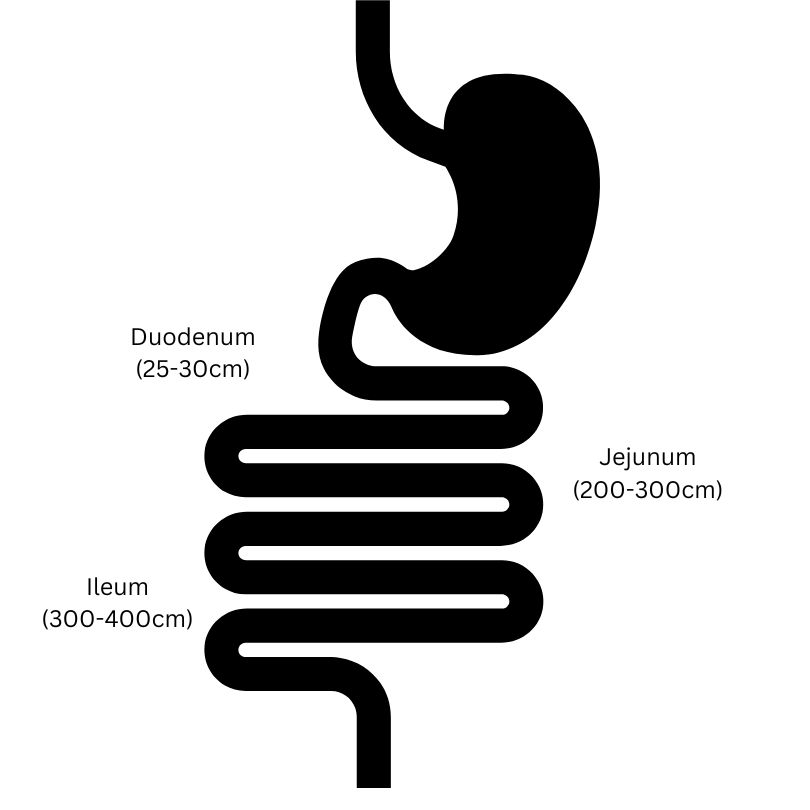
Where is potassium absorbed in the GI tract?
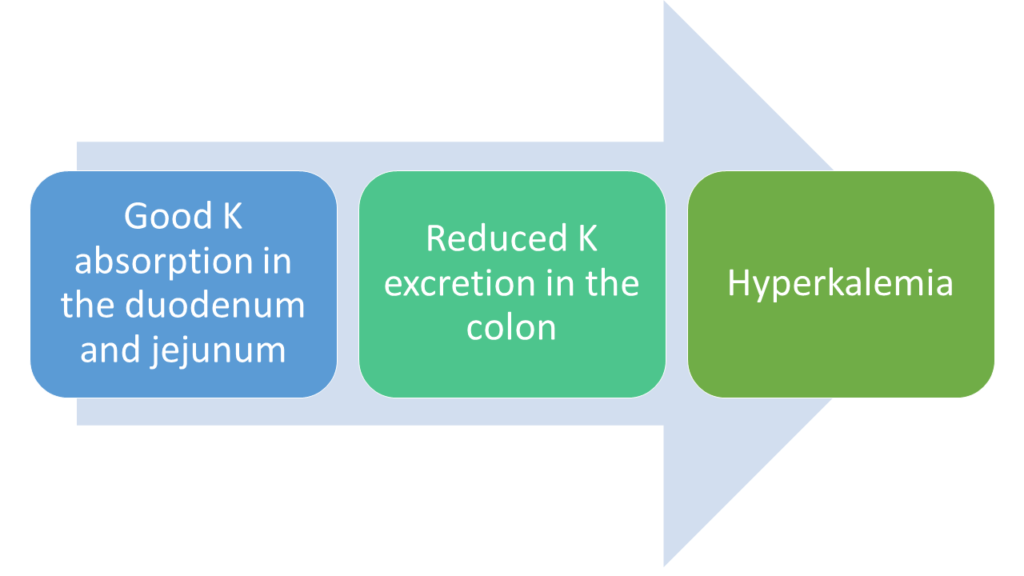
According to this article, potassium is absorbed all along the GI tract, with studies suggestion that potassium is highly permeable across the jejenum and ileum. Furthermore, studies have found that potassium is even more permeable than water when consumed as part of a mixed meal (steak and water). This means that someone with an ileostomy can have high output AND good potassium absorption.
In the general population, the colon is thought to play a small role in potassium balance, absorb or secreting only about 4mEq/day. But, consider that in kidney patients, fecal potassium excretion is increased, so the colon for these patients likely has a large role to play in potassium balance.
So for some patients with ileostomies, they can have good potassium absorption, +/- good water absorption, decrease colonic losses of potassium which results in hyperkalemia.
Take Aways
- Ostomies can be associated with both hypokalemia (more common) and hyperkalemia (less common)
- Hyperkalemia is likely related to a loss of potassium excretion in the colon, coupled with good absorption through the remaining parts of the digestive tract


HI Kelly, thank you so much for this explanation… very embarrassed to say that I have been a renal RD for a long time and I didn’t know this. In fact I do have a pt who has an ileostomy and always high K and I talk to pt/ family every bloodwork… They are considering reversal of ileostomy, so this might be even more of incentive to do so.
Hi Michiyo – thanks so much for your comment! And for sure there is nothing to be embarrassed about! I have been in your shoes exactly. If your patient gets their ileostomy reversed and there hyperkalemia resolves I would LOVE to hear from you!