It’s fat stack Friday. Unfortunately in healthcare, that means I am not talking about a fat stack of pancakes. Fat stack Friday for dietitians means you have a huge pile of blood work referrals to get through and ideally you are going to get them all done today, because otherwise it has to wait until Monday.

So, you aren’t alone when you wonder if you REALLY need to call those potassiums between 5.1-5.5mmol/L. Now, of course no matter the level, its always good to check the trend and you can read more about that here. But for today’s post, I am focusing on the target.
What is a target?
Before I talk about the evidence, I want to take a minute to discuss what a target lab value is. I describe lab targets as the value where I can predict the lowest risk of something bad happening to my patient based on this value.
I used to think of targets as these black and white categories: inside target (good) and outside target (bad). But the truth is that lab values and risk prediction rarely works like that. So let’s take a minute to explore at what potassium levels bad things (for example death) are happening.
At what potassium value does the mortality risk increase?
I really liked figure 2 from this 2021 article that maps out mortality risk against potassium levels by different population groups.
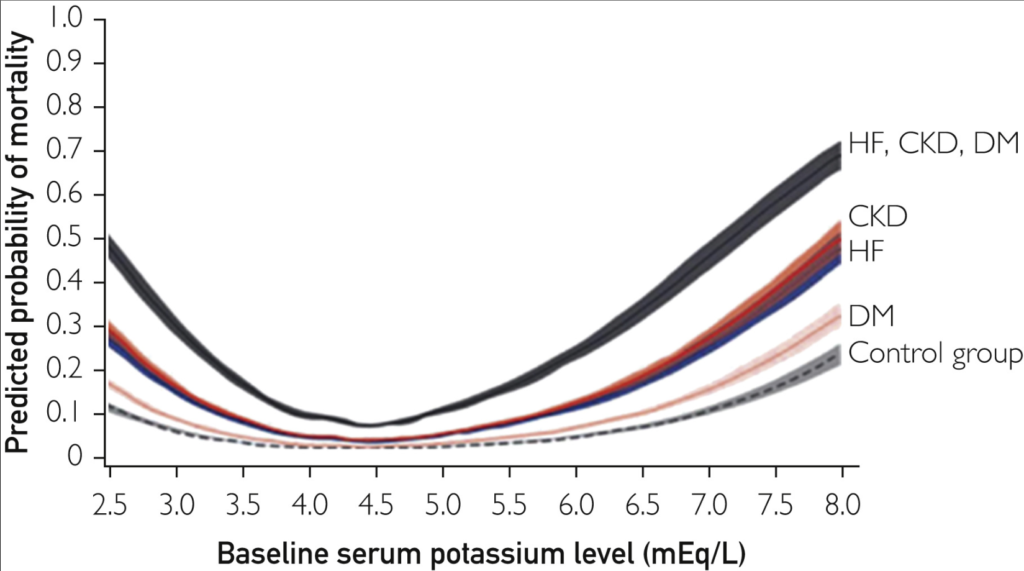
The key things to look at in this image is where is the bottom of the U is. For most of the lines, the bottom of the U falls between about 3.5-5.5mmol/L. Notice that regardless of the serum levels, those with Heart Failure, Kidney Disease and Diabetes have a higher mortality risk than those without (Control Group). And also notice that the mortality risk is increasing at a faster rate for our sickest patients than the mortality risk for our healthiest patients.
How does eGFR impact mortality risk?
In this meta-analysis of over 1.2million people, mortality risk was broken down by eGFR. Here is figure 3B from the article.
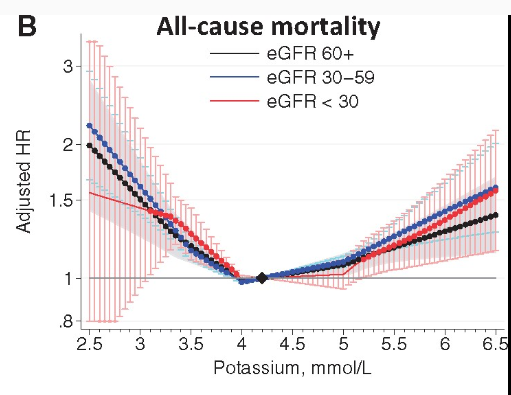
In this study they reported that 4.2mmol/L was the number associated with the absolute lowest risk of mortality. The dots (vs solid line) denote when the risk of mortality became statistically significantly different from the lowest risk point of 4.2mmol/L. Note that for those with a eGFR below 30, the difference in mortality risk doesn’t become significant until 5.3mmol/L.
What’s the target?
The 2020 KDIGO statements of potassium management has a nice potassium classification figure.
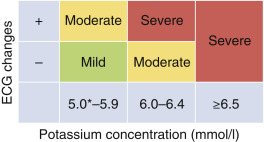
This little table maps out different levels of serum potassium and classifies them into mild, moderate and severe. One limitation for using this is my clinic based practice is I basically NEVER have access to ECGs. But I still like how they group, mild, moderate and severe.
Take Aways
Ok, so back to your fat stack and your K of 5.2mmol/L. Here are my triage tips on whether or not to call:
- Is this a first occurrence? If yes – triage up, if no – triage down (this going back to trend!)
- Does your patient have diabetes? If yes – triage up (higher risk of bad outcome), if no – triage down (lower risk of bad outcomes)
- Is the eGFR under 30? If yes, triage down (lower risk of bad outcomes under 5.3mmol/L); If no, triage up (high risk of bad outcomes).
If you decide you need to call, make sure you use my hyperkalemia assessment to guide you through.