My first position in renal nutrition was in hemodialysis and I started that job in 2010. My second position in renal was in a pre-dialysis kidney care clinic, which I started in 2015. In neither of those jobs was the dietitian responsible for managing acidosis. But now, in my current clinic, it is a dietitian job.
So what does the literature say about nutrition management of acidosis? Let’s take a closer look at today’s article: Nutritional Approaches for the Management of Metabolic Acidosis in Chronic Kidney Disease
What is acidosis in CKD?
The kidney’s play a major role in maintaining the acid-base balance of the body. They do this by:
- Excreting excess anions
- Excreting excess acids
- Neutralizing acids
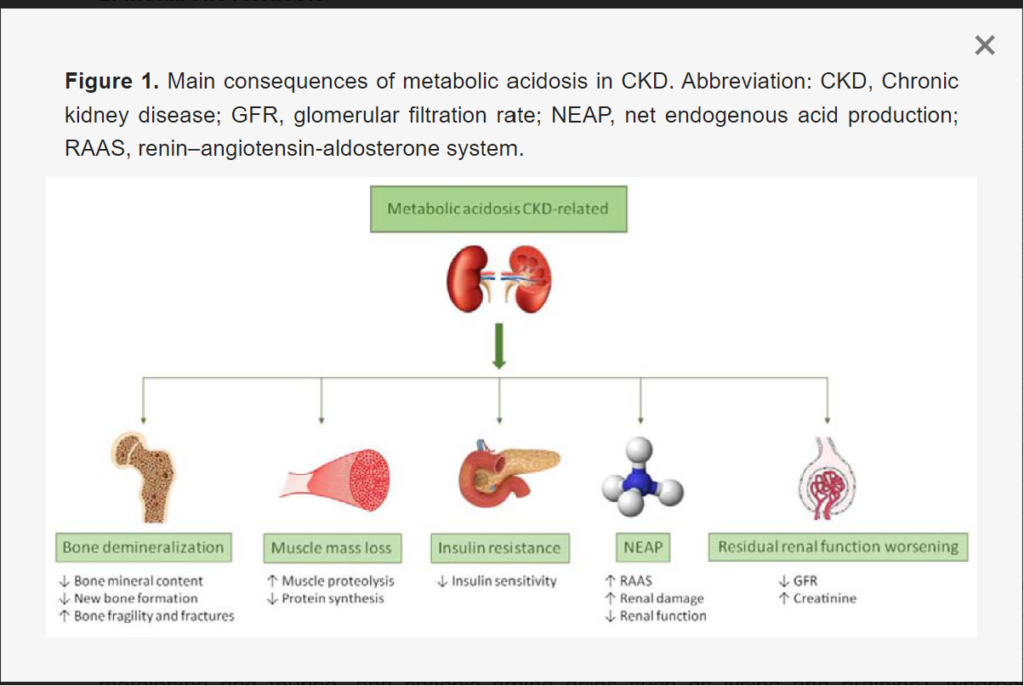
When kidney function declines, the maintenance of acid-base balance can become compromised. This can several detrimental health impacts, as shown in Figure 1 of today’s article.
What foods are acid producing and which are base producing?
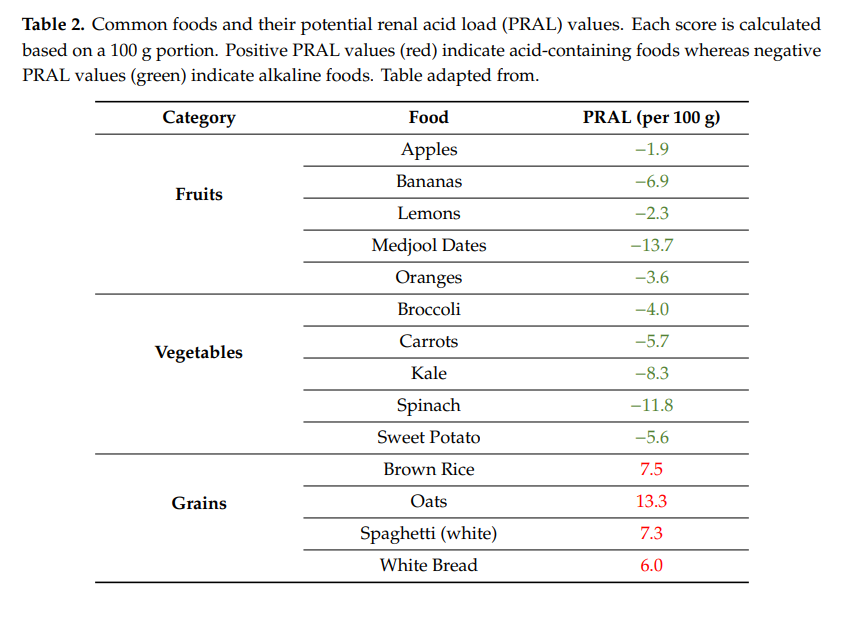
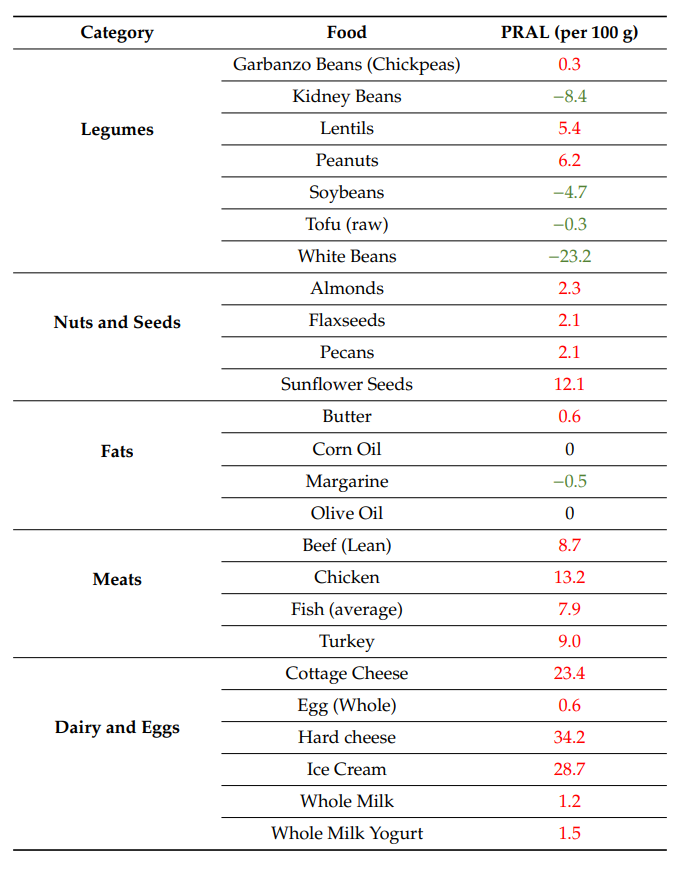
Different foods are thought to have a net acid producing effect, while others are considered base inducing. Animal foods are more likely to be acid producing, where as fruits and vegetables are base producing.
I frequently see these two acronyms in relation to acid/alkaline foods:
- NEAP – standing for Net Endogenous Acid Producing
- PRAL – standing for potential renal acid load
Can diet changes improve acidosis in CKD?
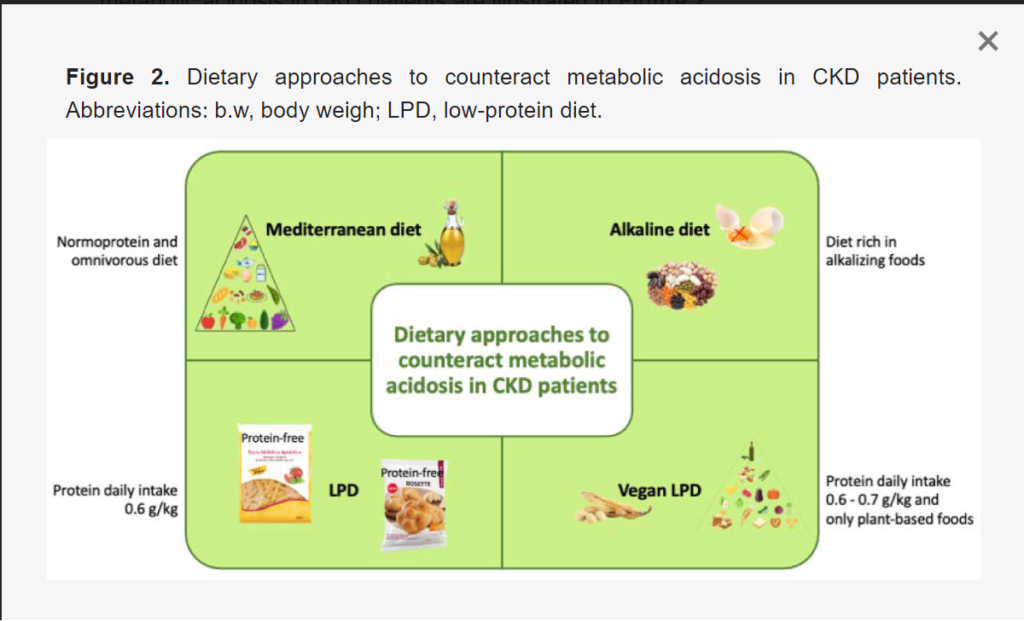
The authors highlight four main nutrition strategies that can help improve acidosis, including a Mediterranean diet, an alkaline diet, a low protein diet and a vegan low protein diet.
The authors recommend these specific steps for patients to follow a more alkaline diet:
- Highlight for patients that vegetables such as kale, broccoli, brussel sprouts, cabbage, onions, garlic, celery, zucchini, lettuce, cucumber, radish, bell pepper, rocket, and sprouted seeds are all encouraged because of their negative PRAL.
- Advise patients to include:
- two portions (about 250 g per day) of the above-cited vegetables in two meals per day
- two portions of fruit (about 300 g per day) after being reviewed according to serum potassium content
- legumes such as lentils, beans, and chickpeas as an alternative source of protein instead of meat
- meal/grain foods such as bread, breakfast cereals, rice, pasta because of their low PRAL.
Take Aways
When I see patients for the first time, they often come with many questions and are highly motivated to make changes to their diet. The renal diet has traditionally been a diet that focused on restriction (e.g. keep your sodium to 1500mg per day and your potassium to 2000mg per day) but this focus is changing.
I also find that sometimes focusing instead on what patients can eat more of, instead of less of can feel more manageable.
I have yet to come across a really great patient handout that outlines which foods are lower and higher in PRAL. If you have one – please share!
But I found this list here:
In your clinics are you teaching alkaline diets? Do patient’s find this helpful or overwhelming? If anyone has experience, I would love to hear about it.



Someone sent me this extensive PRAL list. Thanks so much for sharing! https://www.clinicaleducation.org/documents/revised-summary-pral-list.pdf