In my practice I see a fair bit of hypercalcemia and hypophosphatemia after kidney transplant. But why is this happening and what should I do about it? Keep reading to find out!
According to a 2022 article in the Canadian Journal of the American Society of Nephrology, bone mineral diseases after kidney transplant are common. Though as immunosuppression regimes move away from glucocorticoid therapy, rates are decreasing.
Hypercalcemia – rates and causes
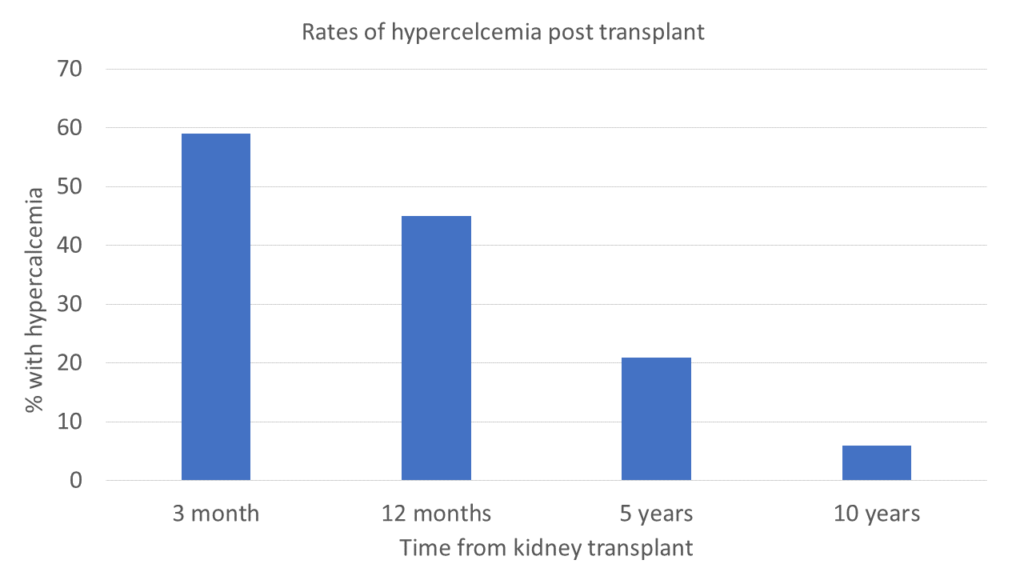
Hypercalcemia is common post transplant. Furthermore, it has been documented at 10 years post transplant. The hypothesized causes of hypercalcemia are:
- Increased urinary calcium absorption related to residual hyperparathyroidism post transplant
- Vitamin D repletion
- Skeletal losses of calcium (calcium leaving the bone and entering the circulating blood supply.
Hypercalcemia can lead to calcification. Calcification is associated with reduced graft survival.
Hypophosphatemia – rates and causes
Hypophosphatemia is common post transplant too. 90% develop hypophosphatemia immediately post transplant and as many as 14% continue with it long term.
The hypothesize causes of hypophosphatemia are:
- High fibroblast growth factor 23 (FGF23)
- Hyperparathyroid induced urinary phosphate wasting
- Immunosuppression medications
But is hypophosphatemia bad?
The authors of this study reported that hypophosphatemia was associated with improvements in both graft survival and reduced mortality. So does that mean hypophosphatemia is good and I should shred those hypophosphatemia referrals?
What do we know about hypophosphatemia?
According to my textbook, hypophosphatemia could be associated with an increased risk of osteodystrophy and fracture risk. However, the authors acknowledged that this phenomenon have been seldom described in the literature.
The 2020 KDOQI guidelines have an opinion based recommendation to prescribe a high phosphorus diet to replete serum phosphate levels. This is an opinion based recommendation because we don’t have any higher levels of evidence support that increased phosphorus intake improves patient outcomes.
Implications for practice
Ok – Hypercalcemia post transplant is not good. As dietitians our job here is pretty simple – we ensure our patients aren’t consuming excessive amounts of calcium, maybe look into vitamin D and then refer back for medical management.
For hypophosphatemia and there are several high phosphorus food lists out there, one from Nova Scotia, another from Alberta. One of the tricky things is considering the bioavailability of phosphorus. If naturally occurring phosphorus found in minimally processed plant foods is bound by phytates and therefore lower in bioavailability, is it effective at increasing serum phosphorus levels? The truth is – that we don’t know.
Dairy products and meat, fish and poultry products are also good sources of phosphorus and likely to be better absorbed. In theory, they would be better at increasing serum phosphorus levels. Though, one could also hypothesize that phosphorus additives in ultra-processed foods would have better bioavailability. Translating to the biggest impact on serum phosphorus levels. Though given the detrimental impacts of ultra-processed foods on health, we would need to ask ourselves:
- Does the benefit of normalizing serum phosphate levels outweigh the potential harm of consuming more ultra-processed foods?
More work to be done
There has never been a study done on the impacts of high phosphorus diet teaching and hypophosphatemia. And there has never been a study done on how high phosphorus diet teaching impacts outcomes such as graft survival or patient mortality.
So the truth is that we do not currently have an evidence-based nutrition intervention for hypophosphatemia management post-transplant. I will go ahead and add this topic to my to do list.
For me, the key questions are:
1) What is the ideal serum phosphorus target post-transplantation?
2) At what serum phosphorus target should high phosphorus diet teaching be initiated?
3) What types of high phosphorus foods (e.g. plant vs animal vs additives) should be encouraged that are associated with meaningful improvements in patients 1) graft survival, 2) mortality and 3) quality of life.


