This is a summary of a presentation I watched at the National Kidney Foundation Spring Clinical Meeting. I was keen to attend this talk to see if there was anything else new to add about how to help patients living with bariatric surgery and CKD after my writing my previous post about this topic.
Speakers: Angela Salas RD, Kellene Isom PhD RD, Kristina Penniston RD PhD
Speaker 1: Basic Bariatric Surgery Overview
Who is a candidate for bariatric surgery?
- BMI above 35 without metabolic complications
- BMI between 30-34.9 with metabolic disease
- For Asian population, suggested thresholds are BMI above 25
It is also ideal to have candidates who are motivated and have social supports.
Who is not a candidate?
- Limited life expectancy
- Active eating disorder
- Pregnant or expecting to be pregnant soon
- Untreated severe psychiatric illness
What are the surgery types?
In 2022, almost 280,000 surgeries were completed in the US.
- 64% sleeve gastrectomy – A laparoscopic surgery that makes the stomach smaller. Better for people who need to take NSAIDs or aspirin or for people with a history of IBS. Preferred surgery for someone wanting to have a kidney transplant. Main contra-indication is GERD.
- 22% gastric bypass – This is both a restrictive (smaller stomach) and malabsorptive (removed intestine) procedure. Post-op patients should be advised never to take NSAID or aspirin after surgery, increased risk of chronic diarrhea/malabsorption
- 9% adjustable band
- 11% revisions
The speaker mentioned that there are other surgeries, there were not discussed in the session today.
What are the nutrition recommendations post op?
- Fluid – A bigger concern immediately post-op. Aim for 1 once every 15 minutes initially after surgery. To help prevent dumping syndrome aim for separation of liquids and solids by 20-30 minutes. Aim for caffeine free, low sugar and non-carbonated beverages.
- Protein – 1-1.5g/kg IBW for BMI 25. Protein shakes are typically required to meet protein requirements for the first 6 months post surgery. Aiming for high quality protein sources, including whey, egg white, casein, milk or soy.
How is diet advanced post-operatively?
- Stage 1: Bariactric clear liquids while in hospital
- Stage 2: Protein based liquids until day 15
- Stage 3: Pureed or blenderized foods, until Week 3-4
- Stage 4: Soft foods, until Week 5-6
- Stage 5: Back to regular diet
What other nutrition concerns may come up after surgery?
Appetite can be decreased post-op. Patients may need to be reminded that they need to eat for nourishment. Each patient’s tolerance can be variable. The goal is to encourage adequate fruits and vegetables, with an initial avoidance of grains. Encourage good chewing and mindful eating.
Common intolerances can include meat, pasta, rice and dairy products.
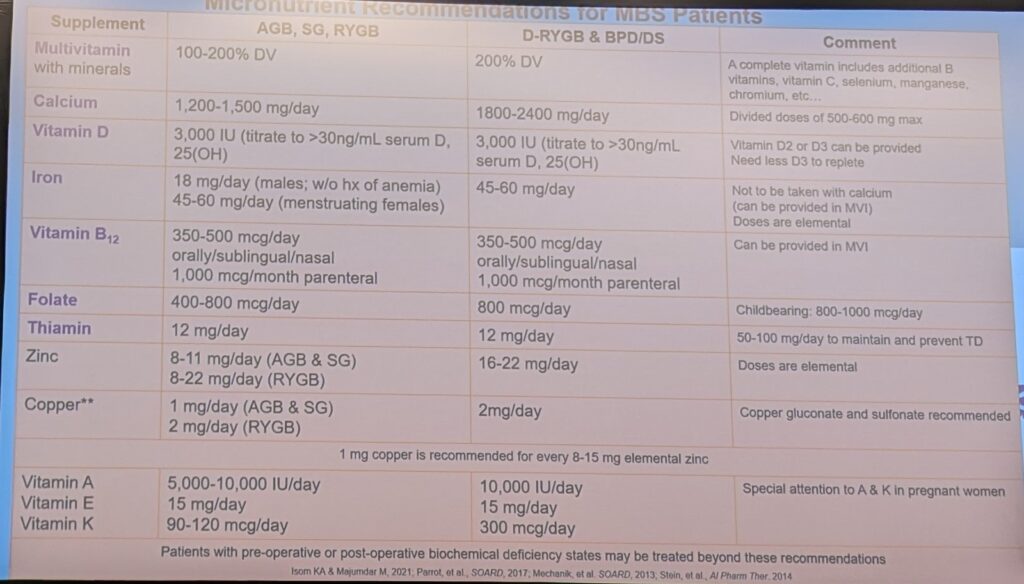
What micronutrient supplements are required post-operatively?
- 2 multivitamins daily for the rest of life
- Take separately from calcium
- Aim for at least 18mg daily of iron
- Calcium aiming for 1200-1500mg daily
- Vitamin B12 500mcg daily or 1000mcg IM monthly
- Vitamin D – based on serum D25 levels, typical maintenance dose is 2000-4000IU daily
- Vitamin A – typically provided in the multivitamin. A question about Vitamin A came up in the Q&A, the panelists stated that they generally don’t use the standard bariatric multivitamins for CKD patient due to concerns with high amounts of Vitamin A. An alternative or other target dose wasn’t provided. To learn more about the importance of Vitamin A in CKD, check out my other blog post here.
Speaker 2: How can nutrition recommendations post bariatric surgery be reconciled for CKD?
Why should people with obesity and CKD consider bariatric surgery?
- Antihypertensive action
- Reduced rates of post-transplant complications
- Reduced risk of CKD disease progression
There is still limited safety data on efficacy of weight-reducing medications in ESKD. There is more evidence that supports the safety of these surgeries in the CKD population.
Do all surgeries have the same risk of micronutrient deficiency?
No. In an increasing order, the band has the lowest risk, followed by the sleeve, the RYGB, and finally the Biliopancreatic diversion, which has the highest risk.
- Sleeve Gastrectomy: top two nutrients at risk are iron and vitamin B12
- Gastric Bypass: Calcium, vitamin D, thiamine and folate
- If there is a distal bypass or if you see a patient with more deficiencies or more bowel movements, suspect there may have been more of the small intestines removed.
Top 5 points to prepare your patient for bariatric surgery
- Preoperative diet – recommended short term pre-operative diet (helps reduce liver size pre-operatively)
- Ensure pre-op micronutrient deficiencies are correct prior to surgery
- Any health eating pattern recommended pre-operatively
- Macronutrients – aim for protein guidelines as per kidney guidelines
- Micronutrient – phosphorus based on kidney guidelines, calcium – aim for adequate DRI, Vitamin D – many patients will be deficient, Iron – may be more likely to be recommended by bariatric team
What are the main nutrition considerations for someone living post bariatric surgery and on dialysis?
- Energy requirements – use MSJ, more accurate in this population.
- Protein – renal and bariatric surgery guidelines tend to agree
- Fluids – there is an increased risk of dehydration post-bariatric surgery
- Iron – may be supplemented post bariatric surgery without iron deficiency anemia
- Calcium and Vitamin D – requirements remain higher post-surgery. Typical calcium of choice for this population is calcium acetate. Calcium carbonate not recommended by the bariatric clinic and calcium citrate not recommended by the renal teams.
- Other micronutrients – the renal multis will meet the water soluble vitamin needs. The concern is the fat-soluble vitamins.
What are the main nutrition considerations for someone living post bariatric surgery and who has received a kidney transplant?
- Protein – guidelines agree
- Energy – this population tends to eat fewer energy
- Malnutrition – may occur and the renal team may need to remind the bariatric team to look out for this
- Copper and Zinc ratio – ensure patients are taking copper if they are taking zinc.
- Follow up – Transplant is not recommended for the first 6-12 months after bariatric surgery
- Magnesium – monitor for this post-operatively, more of a concern on the transplant side than the bariatric side
Special population: pathophysiology of stone formation post-bariatric surgery
There is a small subset of the bariatric surgery patients who will develop kidney stones after surgery. This talk is specific to this population.
Different surgeries have different effects on the urine:
- Bicarbonate wasting – lower urine citrate, overly acidic urine; May be more likely to be seen in the setting of diarrhea. Primary concern is calcium oxalate stone risk.
- Extra-renal fluid losses – lower urine volume, higher super saturation of urine which increases the risk of precipitation increases the risk for all stone types
- Mineral malabsorption – lower urinary magnesium excretion, low urine magnesium is a good indicator of magnesium status, blood magnesium is not a good indicator of magnesium status
- Fat malabsorption – higher urine oxalate
What is the link between calcium intake and calcium oxalate stone formation?
Calcium intake is good for preventing calcium oxalate stones. This is because calcium binds oxalates in the gut and lowers oxalate absorption.
If calcium intake is insufficient for the oxalates in the diet then this the major problem. Often it isn’t about reducing oxalate but increasing calcium. Though they need to co-incide in the gut. Calcium needs to be eaten (or taken as a supplement) at the same time as dietary oxalates are consumed.
Why can there be an increased risk for stones post bariatric surgery?
Any surgery that increases the risk of dehydration or reduced calcium can increase the risk of stones. Hyperoxaluria is the concern for stones. The more weight loss typically the higher the hyperoxaluria.
Where do oxalates come from?
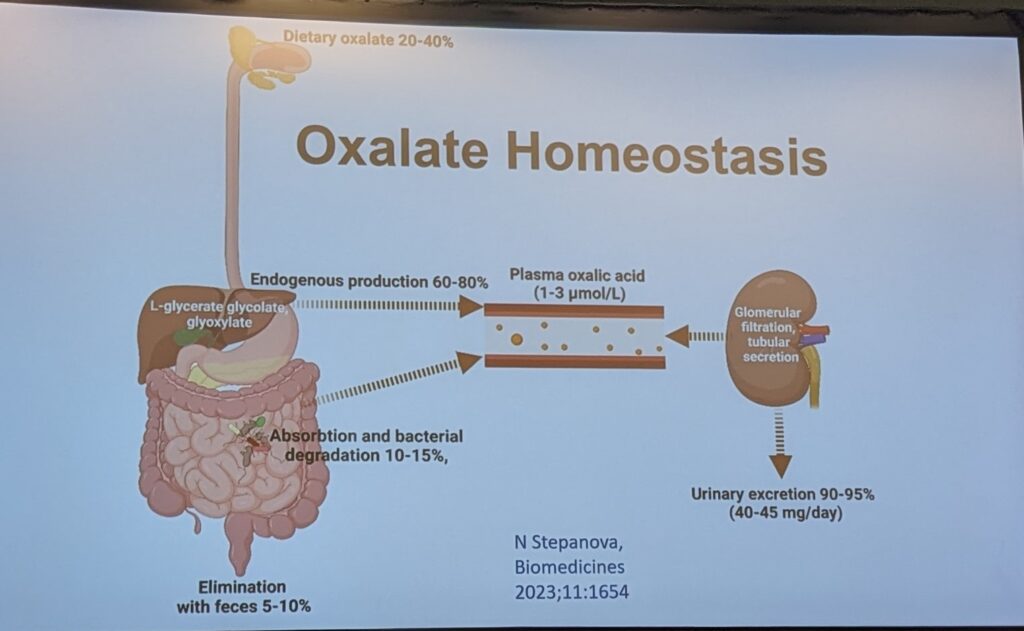
Oxalates can come from diet, but it can also come from genetic mutations were the liver increases oxalate production.
If the source of oxalates is the diet, consider that oxalates occur in many healthy foods. Plants use oxalates to help store calcium or they accumulate it from the stool. High oxalate foods are also high in magnesium and good for gut bacteria. So the key isn’t to reduce oxalates but to reduce the absorption of it.
Diet + Endogenous Production = Oxalates into the Urine
What is the link between the microbiome and kidney stones?
When calcium binds with oxalates in the gut they aren’t absorbed but instead excreted in the stool. As these compounds pass through the colon, the gut microbiota have a chance to ferment and use these compounds. It has been shown that the gut microbiota like to degrade oxalates to be used as a food source.
With the gastric bypass surgeries, a portion of the intestines is bypassed and this can impact the gut microbiome. Given what is known about the physiology of the sleeve, this should be less pronounced, though there is less evidence here.
Why do people develop hyperoxaluria?
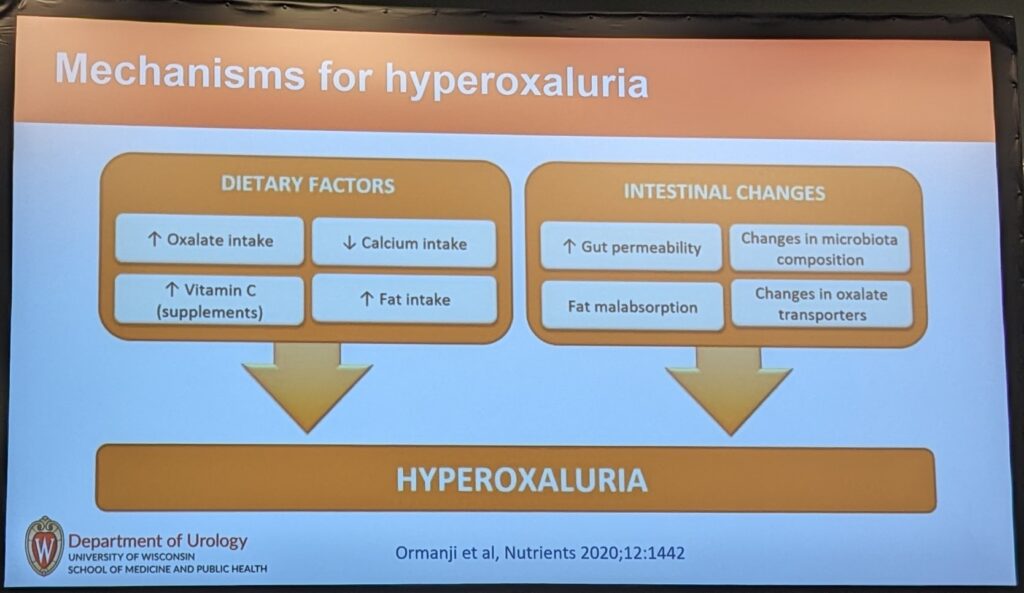
Especially post bariatric surgery where intakes are low, it is unlikely that the causes is excessive oxalate intake. The most likely cause is inadequate calcium intake. The second most likely causes is excess vitamin C supplementation. High vitamin C will result in high oxalate formation.
Why is fat intake associated with stone formation?
The slide notes that high fat intake increases the risk of hyperoxaluria, again the speaker notes that this is unlikely post bariatric surgery. The link here is that fat can bind with calcium in the gut to form soapy compounds that aren’t degraded. When the calcium is bound to fats, it can not bind to oxalates.
How do intestinal changes post bariatric surgery impact the risk of stones?
- Changes in the microbiome, reduced oxalate degradation increasing urine oxalates
- Increased intentinal permeability – once oxalate is in the blood supply it needs to be excreted as humans do not store oxalates in any way
Is diet always the cause of hyperoxaluria?
No. Not all high urine oxalates are associated with diet oxalate consumption or other diet changes. Rat studies have suggested that high urine oxalates may occur even if the rats are feed oxalate free food. This suggests there could be other biological mechanisms that are causing hyperoxaluria
Important point: If higher oxalate consumption isn’t causing hyperoxaluria, then no amount of restriction or calcium binding will help.
How do you prevent stones?
Address the specific urinary stone risk factors:
| Urine Finding | Recommendations |
| Hyperoxaluria | Calcium sources or supplements with meals – chewable, calcium carbonate forms are best. How much calcium should you give? There is not specific amount. But the more oxalates consumed, the more calcium is needed. Starting doses may be around 300mg per meal. The goal is to see urine reductions of oxalates. Lower fat consumption if high May try probiotic formulations contain at least 10 different strains (less evidence for this) Eliminate supplements that may be contributing – e.g. vitamin C, turmeric, cinnamon or other herbals (made from plants are more suspicious for oxalate sources) |
| Hypocitraturia or overall acidic Urine | Bicarbonate repletion |
| Hypomagnesuria | Oral Magnesium repletion – suggested doses were very high – as much as 400-500mg daily may be needed |
| Low Urine Volume | Can be very difficult to address post bariatric surgery, may need to prioritize other prevention strategies. Of note, those who are anuric don’t tend to form kidney stones as they no longer produce urine. |