As a continuation of my 2024 KDIGO Guidelines series and my Low Protein Diet Series – this post will go over what the guidelines have to say with regards to protein.

What are the recommendations?
There is 1 recommendation and 3 practice points related to protein intake:
Recommendation 3.3.1.1: We suggest maintaining a protein intake of 0.8 g/kg body weight/d in adults with CKD G3–G5 (2C).
Practice Point 3.3.1.1: Avoid high protein intake (>1.3 g/kg body weight/d) in adults with CKD at risk of progression.
Practice Point 3.3.1.2: In adults with CKD who are willing and able, and who are at risk of kidney failure, consider prescribing, under close supervision, a very low–protein diet (0.3–0.4 g/kg body weight/d) supplemented with essential amino acids or ketoacid analogs (up to 0.6 g/kg body weight/d).
Practice Point 3.3.1.3: Do not prescribe low- or very low–protein diets in metabolically unstable people with CKD.
Practice Point 3.3.1.5: In older adults with underlying conditions, such as frailty and sarcopenia, consider high protein and calorie dietary targets
What additional information is provided to support these recommendations?
KDIGO is recommending protein intakes in line with the WHO guidelines for protein. They highlight that high protein intake may associate with kidney damage. Why? There are no storage sites for protein. In the body, extra protein is broken down. The protein breakdown products include urea and other uremic toxins.
How does body weight impact protein recommendations?
The KDIGO guidelines are silent on whether to use actual or ideal body weight to calculate protein requirements for adults with a BMI above 25.
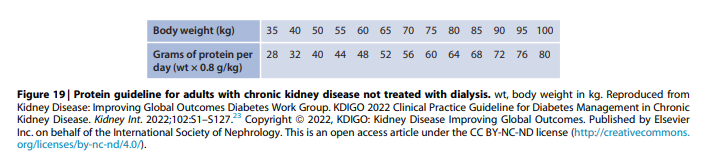
Figure 19 is a table showing body weight and grams of recommended protein. This table includes weights all way up to 100kg. I thought it was interesting that this table reached a high weight of 100kg. A person would need to be taller than 200cm or 6ft 7inches before they had a BMI under 25 with a body weight of 100kg.
What type of protein is recommended?
With regards to protein type (plant vs animal) – KDIGO reports that protein type may also be important. They highlight that observational studies have reported slower eGFR decline with higher plant protein diets. They also state that determining if this is related to protein or lifestyle factors associated with vegetable protein intake is difficult. However, the guidelines highlight that there is biological plausibility. Plant protein diets associate with reduced renal plasma flow, increased renal vascular resistance and lower fractional albumin clearance.
What about very low protein diets?
The 2020 KDOQI guidelines recommend low protein diets. KDOQI graded the evidence used to make this recommendation as Level 1A. The highest level!
However, KDIGO states that there is insufficient evidence to support low protein diets (0.4-0.6g/kg) for slowing disease progression. Citing two meta-analyses which failed to demonstrate reduced deaths or dialysis starts for those in the low protein diet arms. T
They also highlight that most studies investigating low protein diets occurred prior to the availability of RAASi and SGLT2 therapies. We do not know if people on these therapies benefit from low protein diets.
However, very low protein diets, with “strict supervision” may improve kidney outcomes. Though the noted limitations of keto-analogues is high pill burden and high cost.
Are low protein diets recommended in older adults?
Older adults with underlying conditions, such as frailty or sarcopenia, may be exempt from protein and energy restrictions. The KDIGO group recommends setting protein and energy targets for old adults based on the most pressing clinical concern. They highlights that geriatric guidelines recommend protein intakes of 1.0-1.2g/kg to prevent malnutrition and sarcopenia.
If the main concern is old age, functional or nutritional status, following the geriatric guidelines is likely more appropriate.
Take Aways
The 2024 KDIGO guidelines are taking a more relaxed approach to protein restriction than the 2020 KDOQI guidelines. They are also highlighting the importance of considering when more pressing nutrition concerns should take precedence.