Imagine a world where checking your potassium levels is as easy as checking blood glucose levels. What would that do for our understanding of how diet impacts serum levels? Industry and science at hard at work to develop this technology and it may be closer than we think!
Thank you to my friend of mine for putting this on my radar! Because, today I am summarizing this article, which provides a summary of point of care and self-testing technologies for potassium.
Types of potassium monitoring
This article covers a few different types of potassium monitoring options. Some can be done in a person’s home and others that can be in a clinic.
The main ones they discuss are:
- Point of care devices (tests done in a clinic/at the bedside)
- Remote measurement devices
- At home measurement devices
- Urine potassium measurements
- Wearable sensors for interstitial fluid and sweat

Point of care devices
Currently, there are two point of care devices approved for clinic use in America. One of the main concerns with these devices is the large amount of blood required for per sample. Obtaining a large enough drop of blood from a finger stick is challenging. And consider, that any amount of squeezing could result in hemolysis and provide inaccurate results.
Remote Measurement Devices
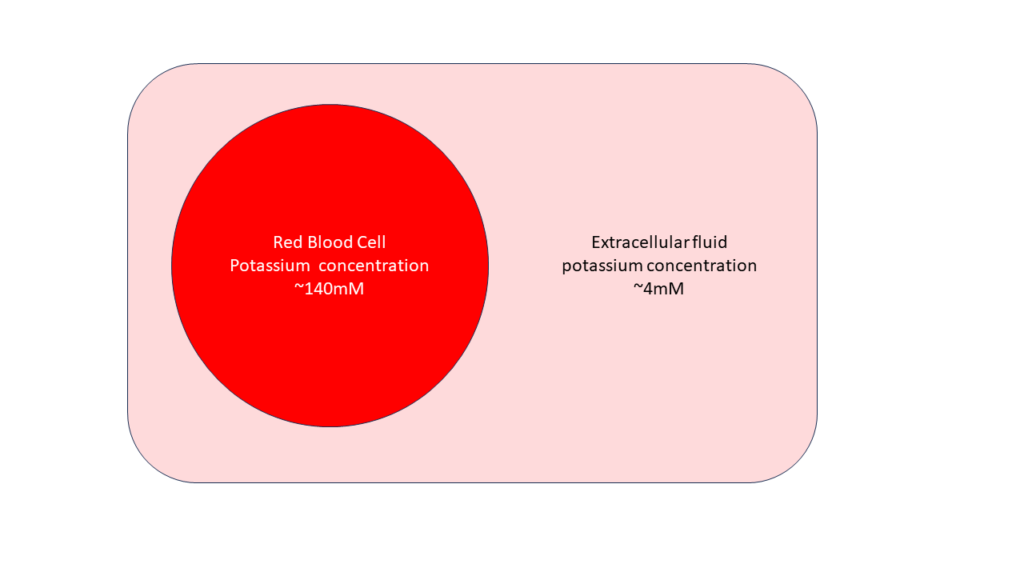
The main concern with these methods is the changes in potassium levels as blood sits. So even if there is a way to procure a large enough sample of blood, how do you preserve the sample? As time can make potassium values change. This is because it takes energy to maintain the potassium concentration gradients within the red blood cells. As energy (glucose) is exhausted, potassium will leak out of the red blood cells. This increases the potassium in the extracellular fluid as the sample sits. Additionally, platelet activation releases potassium, so any blood clotting will also mar results.
At Home Measurement Devices
Six companies have made it publicly known that they are working to develop at home potassium measurement devices. Of these, 2 companies are in the USA, 1 in the UK, 1 in France, 1 in the Spain and 1 in Austria. For more, the goal is to use a test-strip and meter system, similar to a blood glucose monitor. One of these companies is in the clinical testing phase. No launch dates have been released for any company.
Urine Potassium Measures
Several promising scientific results have demonstrated that various technologies can be used to determine potassium in the urine from a spot sample. While this could have clinical validity for understanding potassium movement from the body, it is important to note that urine potassium is not a suitable biomarker of serum potassium.
Wearable potassium measures

- Interstitial fluid – This technology is under development in chicken and pig skin models. Early studies suggest that a sensor could be worm for 24 hours without adverse effects on skin cells. A company in Canada is currently working on this technology. But first, interstitial potassium levels will need to be correlated with serum potassium levels. Plus, we need an understanding of the lag time between the fluids. However, if this technology gets developed the advantage of not worrying about hemolysis and reduced pain makes this an exciting option.
- Sweat potassium – Several sensors have been tested for measuring potassium in sweat, with good effect. The utility of these devices will likely be more for athletes as opposed to having clinical utility. This is because it has already been demonstrated that sweat potassium does not reflect serum potassium levels.
Outstanding Considerations brought up the authors
- Accuracy: it has taken 20 years for blood glucose monitors to get within 20% accuracy for measuring glucose. Potassium is maintained within a tight physiological range. This means that potassium meters will need likely need to read within 0.5mmol/L of the actual levels. Or else they won’t have good clinical utility.
- Time to measurement: given the risk of potassium movement outside of the cell and hemolysis delayed potassium testing could result in psuedohyperkalemia. This means that at home devices will need to be quick at measuring potassium levels.
- Sample collection technique: will need to be excellent due to the risk of hemolysis with any level of squeezing. (As someone who works in diabetes I can see this being a huge problem!)
- Cost: Technologies will need to be affordable for patients and the healthcare system. BG testing in Canada is still cost-prohibitive for many. I can see this being a huge hurdle when the time comes.
What’s the timeframe?
None of these devices have received regulatory approval, but the authors report this could start happening within the next few years. Wouldn’t that be a fun Christmas present?!?