
In my hunt down the rabbit hole about low protein diet’s last week, I reached out to a colleague of mine about low protein diet. She shared this article with me from Australia that commented on the 2020 KDOQI updates.
The Article
In this article, the authors highlight the concern that restricting protein may make it more challenging for patients to consume adequate energy and put them at increased risk of malnutrition. What I also found interesting was the authors comment that:
Consideration should also be given to the potentially negative impacts of intensive protein restrictions on patient quality of life
Lambert et al
What evidence informed this statement?
I think all practicing dietitians are aware that therapeutic diets, regardless of them being for kidney disease, diabetes or celiac disease, can have significant impacts on patient’s quality of life. It’s something that we hear from our patients all the time.
But it got me wondering, what evidence did these authors use to make this statement? Who is this author? (You can see my head plummeting down, down, down this tangential path).
Well, Kelly Lambert is a pretty big deal. She is PhD RD from Australia, who unfortunately I don’t have the pleasure of knowing, but she has done some incredible research on the impacts that renal diets have on patient’s quality of life. In her article “How do patients and carers make sense of renal dietary advice?” she describes the research she conducted by interviewing 26 adults living with chronic kidney disease and asking them about their experiences learning about the renal diet. The main themes she reports are:
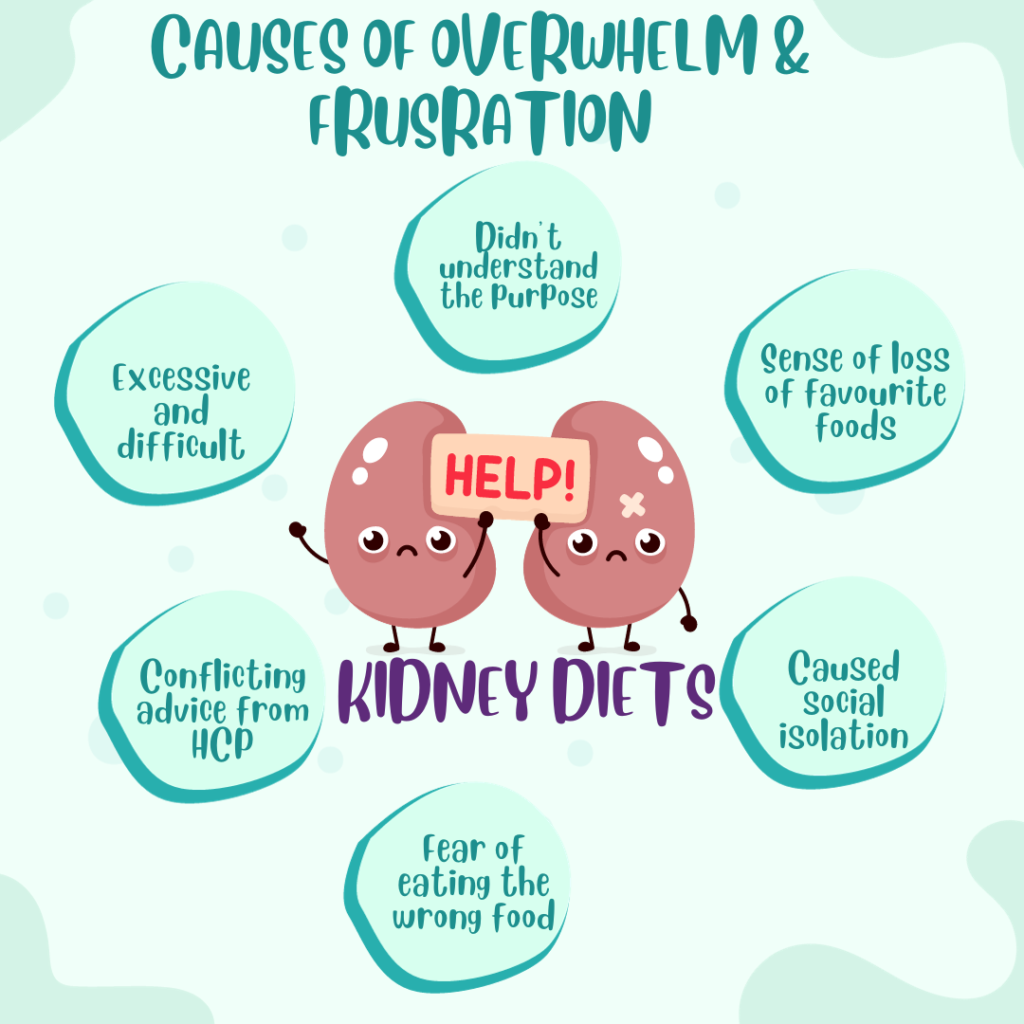
Renal diets are overwhelming and frustrating
The main causes of overwhelm and frustration are highlighted in the graphic below.
Renal diets are complex and challenging
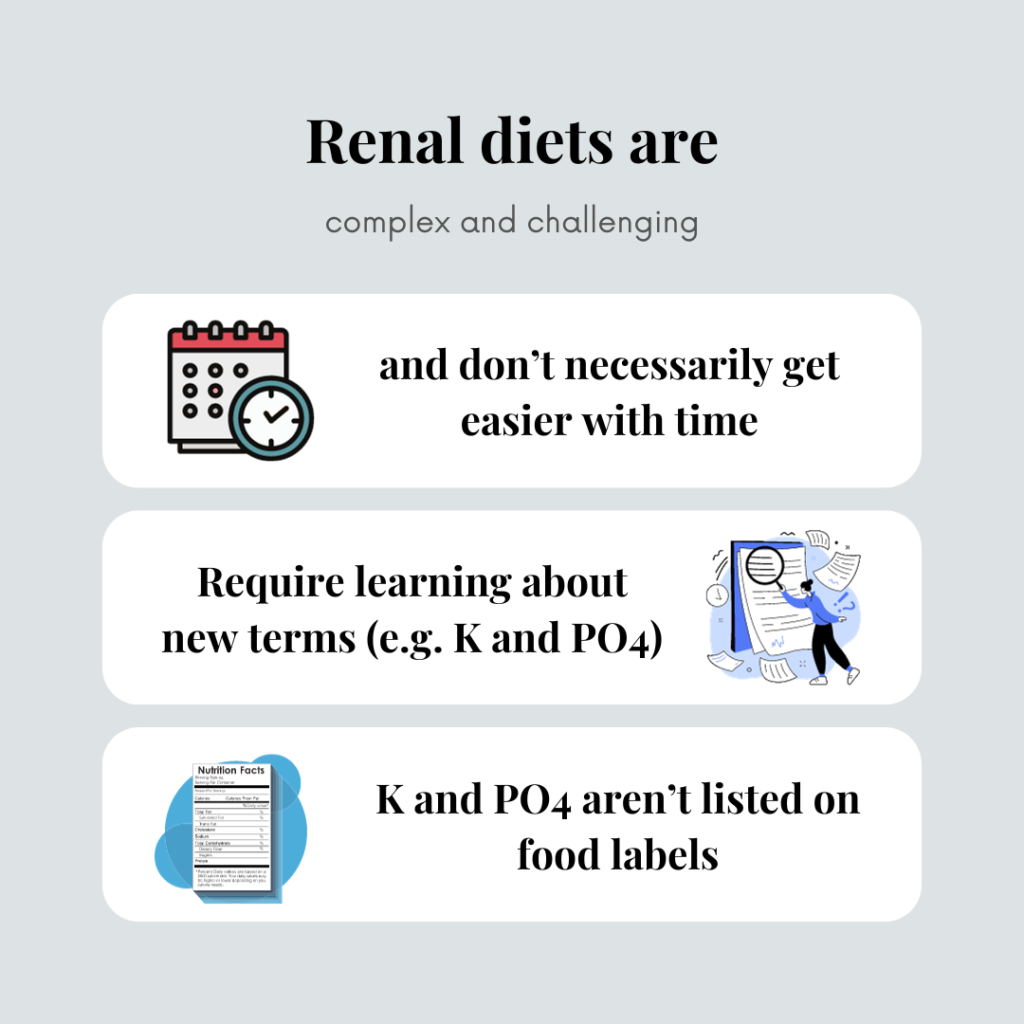
And you may be thinking – well at least potassium is on the food labels in Canada and the US now. Though check out my concern with potassium accuracy on food labels here.
So is it all bad? Do renal RDs cause nothing but negative emotions for our patients?
No, it’s not all bad. The article goes on to state that patients can move beyond feeling overwhelmed and frustrating and learn to accept that following the diet was good for their health and had benefit.
Take Aways
The whole topic has my brain spinning. As dietitians we don’t want our patients to feel overwhelmed or frustrated with their diets – our goal is to help. And yet, if our patients don’t follow the diet this could make life worse if it makes them get sicker.
And just to link back to the idea of low protein diets – for some patients, whose main priority is to prevent starting dialysis, then maybe the more restrictive diet is worth the initial overwhelm and frustration. Though, certainly for other patients low protein diets may just increase their sense of overwhelm and loss and increase disease burden.
So, I suppose, that’s why we do the work we do as dietitians. We work our hardest to match the right diet intervention with the right patient.



One thought on “How do patients make sense of renal dietary advice?”