Danielle from BC asks: “What is the current evidence for protein limits to delay decline in kidney function?
My answer
My first stop to answer a question like this was to look at the 2020 Kidney Disease Outcomes Quality Initiative (KDOQI) Nutrition guidelines. Screen shot below.
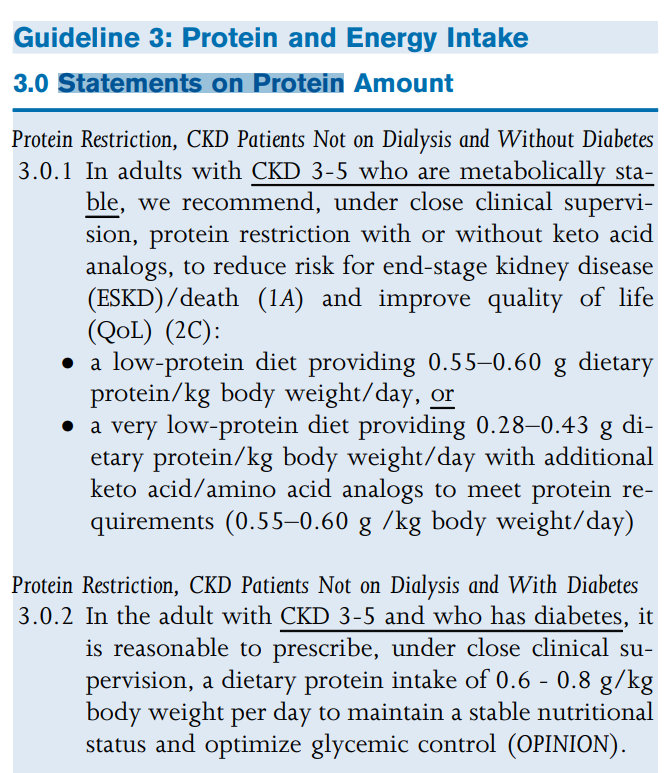
Level 1A Evidence that low protein diets delay risk of ESKD
Ok, so lets look a little closer at the evidence that they used to make that call – because Level 1A is pretty strong evidence.
5 randomized controlled trials looked examined the impact of low protein diets (0.55-0.6g/kg) on the risk of reaching dialysis. 3 of these studies reported reduced risk of reaching dialysis. The study duration was 3-48 months.
Pooled together, results from the secondary analysis of the number of events of death/
KDOQI 2020 Nutrition Practice Guidelines
ESKD combined from the 3 studies indicated a beneficial effect of protein restriction on death/ESKD (OR, 0.621; 95% CI, 0.391-0.985).
Let’s take a closer look some numbers
| Reference | Study Description | Number reaching ESKD/50% reduction in eGFR or Death in Low protein | Number reaching ESKD/50% reduction in eGFR or Death in Higher Protein |
| Locatelli et al, 1991 | 226 patients advised to follow 0.6g/kg protein vs 230 patients follow 1.0g/kg; Followed over 2 years | 29/226 | 45/230 |
| Cianciaruso et al, 2009 | 423 patients advised to follow either 0.6g/kg or 0.8g/kg and followed over ~3 years | 64/212 | 67/211 |
| Hansen et al, 2002 | 82 patients with T1DM randomized to low protein (0.8g/kg) or regular protein (1.0g/kg) | 4/41 | 11/41 |
| 97/479 (20.2%) | 123/482 (25.5%) |
What does this table mean?
The odds of starting dialysis or death were lower with lower protein intake
Combining these three studies shows that 1 in 5 patients in the low protein group started dialysis or died. In the higher protein group 1 in 4 patients started dialysis or died.
What about other outcomes?
Interestingly, protein restriction did not have a clear impact on eGFR alone – though I would argue that this isn’t a great marker because while patients and clinicians look at the eGFR, ultimately we are tracking it because of its ability to predict starting dialysis. At the end of the day, if my patient is still feeling well and delaying dialysis start then this is likely a more important outcome than what their actual eGFR is.
They also looked at quality of life – and I think as dietitians we are always acutely aware of the impact that therapeutic diets can have on quality of life. Specifically, I think we worry that if we restrict someone’s diet too much that this will negatively impact their quality of life. In one study that looked at this, those on a low protein diet actually had better health related quality of life scores than those who weren’t on a low protein diet. Though of course, those tools don’t ask them stuff like: Are you still able to eat and enjoy eating with your friends and family (or some other equivalent question)?
What weight should I use to calculate the protein prescription for my patient?
KDOQI states that the weight used to calculate the prescription will depend on the patient, their health status and their goals and that clinicians should use their clinical judgement.
In clinical practice I will typically use an ideal body weight of a BMI of 25 for adults under age 65 and a BMI of 29 for adults over the age of 65 if the BMI is above these thresholds. Otherwise, I typically calculate the protein prescription using actual body weight.
Take Aways
- KDOQI recommends limiting protein intake to delay progression to dialysis or death
- Even on a low protein diet 1 out of 5 patients will likely reach dialysis or death
- But thats better odds than the 1 out of 4 patients on a regular or higher protein diet
So – my clinical advice. Talk to your patients about this. Give them the odds and have a frank discussion about the pros and cons of trying a lower protein diet.
For some patients, this might be a good option. For others – they may have bigger fish to fry. But all we can do is help them make informed decisions.
Wait – what about very low protein diets and ketoanalogues
Well, if you are loving learning about protein. Check out the next post in this protein series here.
Wait – what if I am worried my patient’s aren’t eating enough?
Well, I got an answer for that too. Check it out here.
Hope this helps! Thanks for the question Danielle!


5 thoughts on “Does limiting protein delay kidney function decline?”