This is part of my Low eGFR in Athletes series – a series of post exploring different reasons why an athlete may have a low eGFR.
In today’s post, we are looking at a very common diet pattern recommended for athletes – high protein diets. Today’s key reference is:
What is a high protein diet?
First things first, let’s define what we are talking about. The author’s define a high protein diet as protein intake above 1.5g/kg per day or greater than 15-16% of total energy intake.
Why do people recommend high protein diets?
High protein diets are often recommended to help athletes increase lean body mass, optimize muscle protein balance and improve performance.
In the article, the authors highlight that the International Society of Sports Nutrition recommends: an overall daily protein intake in the range of 1.4-2.0g/kg body weight per day for building and maintaining muscle mass for most exercising individuals. Furthermore, higher protein intake, above 3.0g/kg/day may have positive effects on body composition in resistance-trained individuals.
Where is all this protein coming from?
Athletes are more than twice as likely to take protein supplements compared to non-athletes. And among body builders, 80% report taking a protein supplement. It is important to note that most studies reviewed in this article used animal based vs plant based protein sources.
Why would high protein diets impact kidney function?
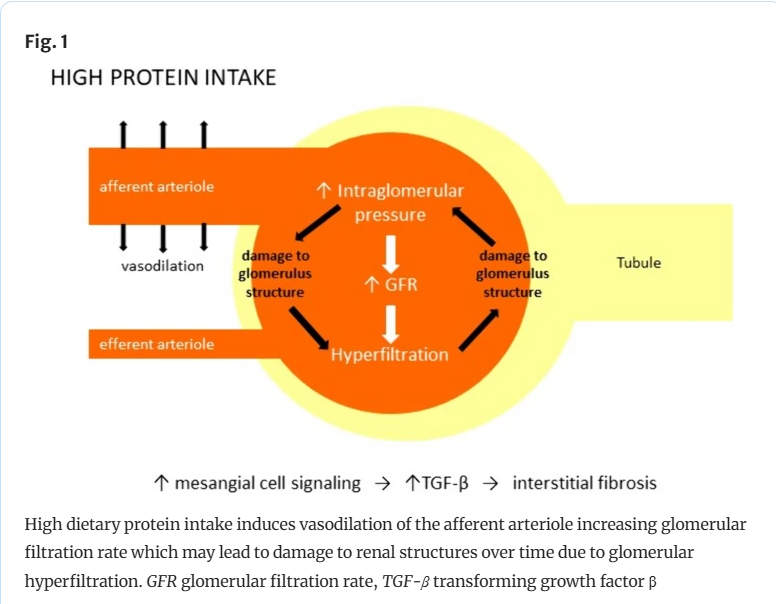
High protein intake increases blood flow through the kidney. This increases the pressure through the glomerulus, meaning the kidney filter more blood to increase the excretion of nitrogenous waste. Nitrogenous waste is a hallmark breakdown product of protein.
What I tell my patients is that we don’t store nitrogen in our bodies, so we need to get rid of it. And that is one of the kidney’s job. Amino acids, which make up all proteins, contain nitrogen (see the image below).
Other potential concerns with high protein intake are:
- Changes in the gut microbiome, leading to a proinflammatory response.
- Higher phosphorus intake leading to stimulation of Fibroblast Growth Factor 23 (FGF23). High FGF 23 can stimulate a cascade leading to increased endothelial dysfunction and oxidative stress.
- Higher dietary acid load, which may promote intrarenal injury
Isn’t better filtration through the kidneys good?
Unfortunately, no. In animal models and clinical trials of people living with kidney disease, this extra filtration through the kidney leads to glomerular injury and scarring. Overtime, this leads to proteinuria and kidney function loss. This is termed hyperfiltration.
So in the early stages, you might see a high GFR (say above 100 or 120) but this indicates hyperfiltration. Hyperfiltration means the kidney is working harder than it should and is at risk of tiring itself out. (See figure 1 below for the more technical over-view provided by the authors).
What studies have researchers conducted in healthy populations?
In 2014 a systematic review and metanalysis compared the impact of high protein vs normal/low protein diets on kidney function in healthy populations. This analysis included 2160 people with an eGFR above 60. This analysis found that high-protein diets significantly increased eGFR by approximately 7. In 2018, a meta-analysis focusing specifically on RCTs reported that high protein intake during a pre/post intervention period led to a non-significant increase in eGFR of 0.11.
What are the critiques of these studies?
De Lorenzo et al emphasize that researchers and clinicians need to consider two important factors when interpreting these studies.
- eGFR: The studies used estimated GFR, as opposed to a measured GFR, which is less accurate in people with normal kidney function.
- Short Duration: Only 6 of the 30 studies were 1 year or more. The median study length was 6 weeks. Kidney damage takes years to occur, short studies are unlikely to capture changes in kidney function related to diet.
What long term data is there?
Several epidemiological studies that have followed participants for many years have reported that those who consume either the highest amounts of total protein or red meat had higher rates of CKD, hyperfiltration, proteinuria or eGFR decline.
What studies have researchers conducted in athletes?
de Lorenzo et al were critical of studies on athletes asserting the safety of high protein diet, arguing that their short duration (last 8-16 weeks) is likely insufficient to understand the long term impacts on kidney health. One study which last for 2 years, only included 5 people, which lacks the statistical power to confirm safety in larger populations. Other studies have failed to use a normal protein diet as a control, which can make comparing changes challenging.
What areas require further study?
The authors highlight several key areas for further study:
- The impact of high plant protein diets, as these may have less negative impact on kidney health than high animal protein diets
- Comparison of normal protein diets as the control with high protein diets
- Using alternate measures of kidney function, such as 24 hour urine outputs for creatinine clearance or GFR using cystatin C.
Take Aways
While the sports community often recommend high-protein diets to improve body composition in athletes, the kidney community remains concerned about the potential long-term impact of such diets on kidney health.
While some studies have last 1 or even 2 years, these studies are likely too short to fully understand how these diets will impact kidney function over the long term.
There is biological plausibility that high protein diets make kidney’s work harder and without good quality long term studies confirming safety, it is unlikely that the kidney community will fully get on board with high protein diets.

One thought on “Are high protein diets for athletes safe for kidney health?”